Co-occurring mental health and substance use disorders trap millions in fragmented, ineffective care cycles.
In 2018, 9.2 million U.S. adults lived with both conditions, yet only 8% received treatment for both.
Atlanta’s integrated dual-diagnosis programs combine hospital-based detox, assertive community treatment, medication-assisted therapy, and housing support to close this gap.
This article breaks down which Atlanta models deliver measurable results, the data behind their success rates, and how to match your situation to the right level of care.
Why Integrated Dual Diagnosis Treatment Atlanta Leads the Nation?
Atlanta’s dual-diagnosis landscape stands out because hospital systems, private PHP and IOP centers, and public behavioral health infrastructure work together across a true continuum.
National guidance from SAMHSA TIP 42 is clear: the best way to serve people with co-occurring disorders is to provide integrated, comprehensive, person-centered services, not operate in silos or use treatments in isolation.
What does that actually look like in practice?
In Atlanta it means Anchor Hospital Behavioral Health System can deliver medically managed detox, inpatient psychiatry, partial hospitalization, and intensive outpatient care under one roof with continuity of psychiatric medication and therapy.
It means The Berman Center can step clients down from hospital PHP into their community IOP while maintaining the same dual-diagnosis clinical team.
It means Dunwoody Recovery Place initiates medication for opioid use disorder during detox and coordinates telehealth follow-up the next day.
Georgia’s 2022-2023 state-level data from the National Survey on Drug Use and Health includes measures for co-occurring substance use disorder with any mental illness and with serious mental illness.
These numbers confirm what providers see: dual-diagnosis cases are common, clinically complex, and require more than standard outpatient counseling alone.
The region’s CARF-accredited outpatient programs accepting Medicaid and Medicare fill another critical gap.
When a patient stabilizes through Anchor’s hospital program, they can transition to Atlanta Recovery Place or CHRIS 180 for ongoing outpatient dual-diagnosis care without insurance disruption.
This cross-payer, cross-setting approach mirrors Certified Community Behavioral Health Clinic standards that require comprehensive mental health and substance use services with 24/7 crisis access, regardless of ability to pay.
What Makes Dual-Diagnosis Programs Effective?
Not all programs calling themselves integrated actually deliver on that promise. Federal treatment guidance and rigorous trials point to six features that separate effective models from marketing claims:
Hospital-based medical detox with psychiatric stabilization. Withdrawal management is the entry point for many people with severe co-occurring disorders.
Evidence-based protocols from SAMHSA TIP 63 emphasize offering medications for opioid and alcohol use disorders at every level of care, including detox.
Anchor Hospital and Peachford Behavioral Health Systems deliver this standard with onsite medical monitoring, MAT initiation, and immediate psychiatric evaluation.
Assertive Community Treatment and Intensive Case Management matched to need. For clients with high complexity like homelessness and severe mental illness, ACT teams provide multidisciplinary support with low caseloads and 24/7 coverage.
The Canadian At Home/Chez Soi trial randomized over 2,000 participants and found Housing First paired with ACT or ICM produced remarkable gains: participants spent 73% of time in stable housing versus 32% under usual care, and 62% were continuously housed in the final six months compared to only 31% in the control group.
Emergency department case management and care plans. A 2023 systematic review of 12 studies found ED-based case management and individualized care plans reduce repeat ED visits among frequent users with mental health issues.
Case management also showed promising improvements in outpatient engagement and some clinical and social outcomes, though evidence remains heterogeneous.
Atlanta’s high-volume EDs can leverage this model to connect people in crisis to Dunwoody Recovery Place detox or Emory Addiction Center IOP within 48 hours.
Medications for opioid and alcohol use disorders embedded throughout. The National Academies’ consensus report confirms medications for opioid use disorder save lives by reducing mortality and overdose risk.
Peachtree Wellness Solutions explicitly offers buprenorphine and naltrexone programs integrated with psychiatric care and aftercare planning. Dunwoody Recovery Place provides on-site MAT during residential stays.
This coordination across detox, residential, PHP, IOP, and outpatient levels eliminates the gap where patients relapse between programs.
Telehealth to maintain continuity and reduce attrition. A 2022 Evidence Brief reviewing telehealth-delivered mental health care found it generally achieves comparable effectiveness and safety to in-person treatment while improving access and retention.
Among U.S. veterans, telehealth utilization was associated with lower risk of buprenorphine discontinuation.
For Atlanta clients juggling work, childcare, or transportation barriers, hybrid PHP and IOP models with virtual therapy groups and medication management keep people engaged when life gets complicated.
Measurement-based care and structured transitions. The Joint Commission recommends routine outcome measurement, and research shows it enhances therapeutic alliance and adherence.
Programs that track symptom scales, days of housing stability, ED visits, and engagement metrics can adjust intensity up or down in real time.
TIP 42 emphasizes that movement across levels of care must not become a barrier to evidence-based services.
Structured handoffs with shared care plans between Anchor Hospital inpatient, The Berman Center PHP, and outpatient MAT clinics exemplify this principle.
Atlanta’s Best Integrated Dual-Diagnosis Treatment Models
Atlanta offers a range of integrated dual-diagnosis treatment options that span the full continuum of care. Below is an overview of how key program types stack up by level of care and access profile.
Hospital-Based Programs with Full Continuum
Several hospital-based behavioral health systems in the Atlanta area provide robust co-occurring treatment within a full continuum of care.
These programs typically offer hospital inpatient, hospital-based detox, partial hospitalization, intensive outpatient, and standard outpatient services, often with medication-assisted treatment (MAT) options for substances such as alcohol, benzodiazepines, cocaine, fentanyl, methamphetamines, and opioids.
Many of these hospital systems hold national accreditations, accept public payers such as Medicaid, Medicare, and TRICARE, and increasingly list telehealth availability.
For medically complex cases, such as severe withdrawal risk, bipolar disorder with co-occurring opioid use, or active suicidality, these end-to-end hospital continuums with broad payer access generally meet the highest standard of medical oversight and safety.
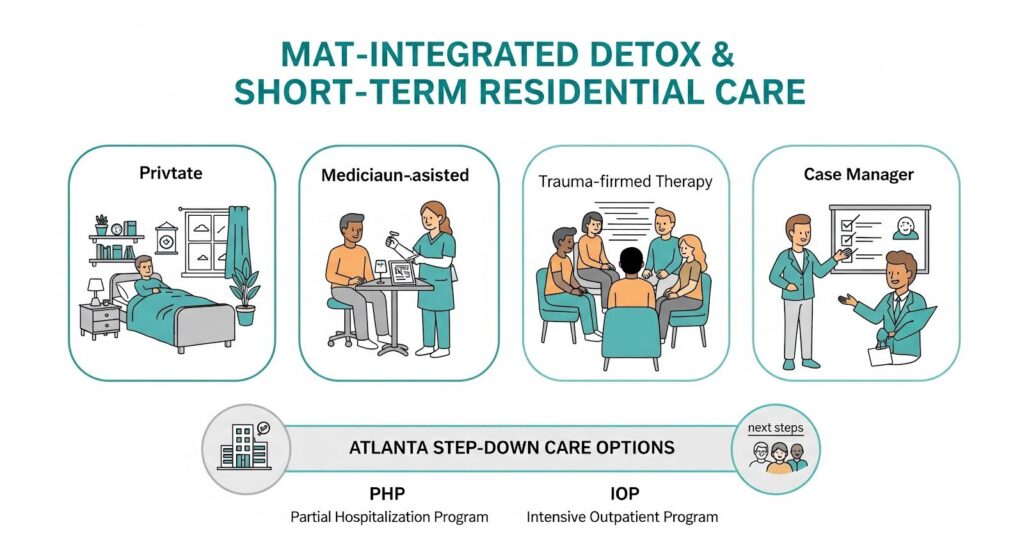
Detox and Short-Term Residential with MAT Integration
Private detox and short-term residential programs serve as important stabilization points for individuals who may not require or prefer a full hospital setting.
These facilities often provide medically supervised detox in smaller, more private environments with on-site MAT and trauma-informed therapy.
Many such centers emphasize immediate access to addiction medicine providers, private or semi-private rooms, and careful transition planning into step-down levels of care such as partial hospitalization (PHP) and intensive outpatient programs (IOP) in the Atlanta area.
For individuals seeking a more discreet or less institutional setting, particularly professionals or those deterred by large hospital environments, these detox and short-term residential programs can function as an effective bridge into longer-term dual-diagnosis treatment.

Strong PHP and IOP Dual-Diagnosis Centers
Specialized PHP and IOP programs form the backbone of ongoing dual-diagnosis care in Atlanta. These centers commonly provide:
- Structured day and evening programming for adults and, in some cases, adolescents
- Individualized, evidence-based therapies such as CBT and DBT-informed groups
- Experiential and family-based therapies
- Regular psychiatric evaluation and medication management
- Clear step-down pathways from PHP to IOP to outpatient care for continuity
Many of these programs also operate prescription drug–specific tracks, including care tailored to benzodiazepine and opioid use disorders.
Access profiles vary: some centers are primarily out-of-network with private insurers and more suitable for those with out-of-network benefits or private pay, while others have broader in-network relationships.
The Summit Wellness Group is one example of a private dual-diagnosis provider offering PHP and IOP for individuals with co-occurring mental health and substance use disorders. Across its Atlanta-area locations, The Summit Wellness Group emphasizes:
- Integrated treatment of addiction and underlying mental health issues
- Evidence-based care informed by CBT and other proven modalities
- Robust group therapy, individual counseling, and family support
- Thoughtful discharge and aftercare planning to support long-term recovery
This type of PHP/IOP model is well-suited for clients who no longer need 24/7 residential or hospital care but still benefit from intensive, structured support.
Public-Payer Accessible Outpatient Programs
Atlanta also has a number of CARF-accredited outpatient and intensive outpatient providers that accept public payers such as Medicaid and Medicare, as well as TRICARE and sliding-fee scales. These programs often provide:
- Outpatient, IOP, and sometimes PHP levels of care
- MAT services for alcohol and opioid use disorders
- Dual-diagnosis capability, including psychiatric support and counseling
Because of their broader financial accessibility, these programs play an important role in equity and can pair well with hospital-based detox and inpatient care for step-down continuity.
Academic-affiliated IOPs and long-standing outpatient centers in the area bring additional clinical oversight and expertise; prospective clients are encouraged to confirm MAT policies and detox linkages during intake to ensure a seamless continuum.
Young Adult Specialists
For young adults, specialized programs offer developmentally personalized dual-diagnosis care. Atlanta has programs that:
- Focus on ages roughly 18 to 28
- Address anxiety, depression, self-harm, suicidality, and substance use
- Incorporate modalities such as DBT, CBT, EMDR, experiential therapies, and intensive family involvement
Some programs hold advanced certifications, such as DBT-Linehan Board of Certification status, which carry significant clinical weight for teens with severe emotional dysregulation and co-occurring substance use.
PHP and IOP options for young adults extend this level of care into less restrictive settings, which is particularly important when psychiatric severity is primary in co-occurring presentations.
Matching Your Needs to the Right Program Level
- Hospital detox plus psychiatric stabilization with Medicaid or Medicare: Start at Anchor Hospital Behavioral Health System; step down to CARF-accredited outpatient programs like CHRIS 180 Inc or Atlanta Recovery Place.
- Private residential detox with on-site MAT: Choose Dunwoody Recovery Place; plan step-down to The Berman Center PHP and IOP or Peachtree Wellness programs.
- Academic IOP oversight for co-occurring care: Choose Emory Addiction Center IOP; verify MAT policy and hospital linkages during intake.
- Adolescent with severe emotion dysregulation and substance risk: Choose Hillside residential if DBT-intensive; Newport Academy or Embark for PHP and IOP day treatment.
- High-need adults with homelessness and frequent crises: Request ACT team referral through ED-based case management; pair with Housing First pathways when available in Atlanta’s public behavioral health network.
Outcome Data That Proves These Dual-Diagnosis Treatment Models Work
National data frames what Atlanta programs can achieve. The treatment gap is stark: half of the 9.2 million adults with co-occurring disorders received no treatment in 2018, and only 8% got care for both conditions. This unmet need drives preventable emergency visits, overdoses, and homelessness.
Programs integrating Housing First with assertive community treatment produce large, durable gains. In the randomized trial, participants spent 73% of time in stable housing versus 32% under treatment as usual.
In the final six months, 62% of Housing First participants were continuously housed compared to 31% in the control group.
These housing improvements enable consistent psychiatric medication adherence, therapy attendance, and reduced acute care use.
ED-based case management and individualized care plans reduce repeat ED visits among frequent users with mental health issues, according to the 2023 systematic review of 12 studies.
Case management also showed promising improvements in outpatient service use and clinical and social outcomes.
While evidence remains heterogeneous and definitions of frequent ED use vary across studies, the directional benefit is consistent and operationally actionable for Atlanta’s high-volume emergency departments.
Medications for opioid use disorder substantially reduce mortality and overdose. ED-initiated MOUD has emerged as an effective model to engage high-risk patients at critical moments.
Telehealth delivery extends access and improves retention: among U.S. veterans, telehealth was associated with lower risk of buprenorphine discontinuation.
A two-year retrospective analysis found comparable treatment outcomes for telepsychiatry versus face-to-face buprenorphine MAT for opioid use disorder.
For Atlanta programs, adopting measurement-based care dashboards that track symptom scales, housing stability, ED visits, and engagement will verify local effect sizes and guide continuous improvement.
Highland Rivers Behavioral Health, a statewide public provider, posts annual reports and program fact sheets demonstrating this transparency standard.
While not Atlanta-specific, their crisis stabilization and detox infrastructure and emphasis on individualized recovery plans with flexible hours model what integrated public systems can achieve.
Why Do Integrated Models Close the Gap?
Dual-diagnosis care fails when mental health and substance use treatments operate in separate buildings with separate teams.
Patients fall through those cracks during transitions, relapse before the next appointment, or give up when insurance requires prior authorization from three different offices.
Integrated programs succeed because one care team manages psychiatric medications, initiates buprenorphine, delivers trauma therapy, coordinates housing referrals, and adjusts intensity based on weekly outcome measures.
When a client at The Berman Center shows worsening depression scores on the PHQ-9, the same team that runs their DBT group can arrange a psychiatry visit within 48 hours and add telehealth check-ins.
When someone at Anchor Hospital stabilizes enough to leave inpatient, the PHP team already knows their medication regimen and trauma history.
This is not theoretical. TIP 42 cites decades of consensus: integrated care improves engagement, reduces relapse, and lowers acute utilization.
The Housing First RCT quantified how much better: more than double the stable housing time. The ED case management review documented fewer repeat crises.
The MOUD evidence established lower mortality. Atlanta has the pieces in place; the work now is connecting them with structured transitions, shared data, and equitable access.
The Bottom Line for Atlanta Families and Providers
If you are choosing a program, ask these questions: Does the facility offer medically supervised detox or direct linkage? Are psychiatric medications and MAT available at every level?
Do they accept your insurance, including Medicaid or Medicare? Can you access telehealth between visits? Do they measure outcomes and adjust your care plan based on results? Programs answering yes to all five demonstrate integration worth trusting.
Atlanta’s dual-diagnosis ecosystem includes nationally recognized hospital systems, evidence-based private PHP and IOP centers, public-payer outpatient programs, and adolescent specialists.
No single program fits everyone, but the region’s layered continuum ensures that high-acuity hospital cases, moderate-need IOP clients, homeless individuals requiring ACT and housing, and teens needing DBT-certified residential care all have access to integrated, effective treatment.
The data backs it: integrated models work. Atlanta’s challenge now is making sure every person who needs this care can find it, afford it, and stay connected across the full recovery journey.
Ready to explore which program matches your needs?
Reach out for a confidential consultation with Summit Wellness Group that integrates evidence-based therapies with personalized support.
