Many people starting Lexapro for anxiety or depression wonder if they can also take Xanax for immediate relief. Combining escitalopram (Lexapro) with alprazolam (Xanax) is possible for short periods under medical supervision, but the pairing introduces additive sedation, dizziness, and impaired coordination that can affect daily activities like driving. This article explains the safety profile, common side effects, and practical guidance to help you make informed decisions with your doctor.
Understanding the Interaction Between Lexapro and Xanax
Escitalopram (Lexapro) is a selective serotonin reuptake inhibitor that treats anxiety and depression by gradually increasing serotonin levels over two to four weeks. Alprazolam (Xanax) is a benzodiazepine that works within minutes to hours by enhancing GABA, the brain’s main calming neurotransmitter.
There is no strong evidence for a direct pharmacokinetic interaction between these medications; escitalopram does not meaningfully inhibit the enzyme that breaks down alprazolam, and alprazolam does not alter escitalopram levels. The primary clinical concern is pharmacodynamic: both drugs depress the central nervous system, and their effects add together, producing heightened sedation and psychomotor impairment.
This additive effect becomes especially important in older adults. Age-related reductions in drug clearance mean that both escitalopram and alprazolam reach higher blood concentrations at the same dose in people over 65. Older adults also experience increased sensitivity to sedatives, magnifying risks of falls, confusion, and cognitive impairment when the two are combined.
Common Side Effects When Taking Xanax With Lexapro
The most frequently reported side effects when using alprazolam and escitalopram together reflect their combined impact on the central nervous system. Patients commonly experience somnolence and daytime sleepiness, particularly after taking alprazolam and during the first weeks of escitalopram therapy. Dizziness and lightheadedness are also typical, especially when standing up quickly or during dose increases.
Impaired coordination and unsteadiness can make everyday tasks like climbing stairs or walking on uneven surfaces hazardous. Many people notice difficulty concentrating, slower thinking, and memory problems, especially for new information learned shortly after taking alprazolam. In vulnerable individuals, particularly older adults taking multiple medications, confusion and delirium can occur.
These effects are most pronounced during the first days to weeks of starting escitalopram, when the SSRI itself can cause dizziness and sedation. Adding alprazolam during this window amplifies the burden, creating a paradox: the benzodiazepine provides rapid symptom relief but simultaneously increases the risk of accidents and impairment.
Table: Patient-Reported Side Effects
| Side Effect | When It Occurs | Who Is Most at Risk |
|---|---|---|
| Somnolence | First days to weeks; after alprazolam doses | Older adults, higher doses, multiple sedatives |
| Dizziness | Early SSRI initiation; dose increases | Dehydration, low blood pressure, polypharmacy |
| Impaired coordination | Shortly after benzodiazepine dosing | Older adults, those with balance issues |
| Memory problems | Hours after alprazolam | High doses, alcohol co-use |
| Confusion | Any time with vulnerability | Advanced age, infection, multiple medications |
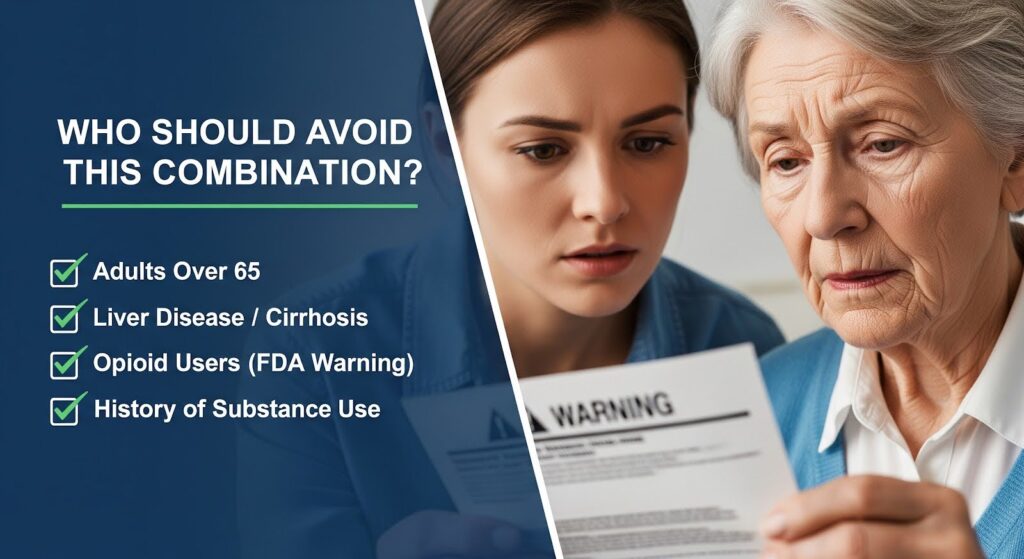
Who Should Avoid This Combination?
Certain groups face substantially higher risks when combining these medications. Adults over 65 should generally avoid alprazolam due to increased sensitivity and reduced clearance; if a benzodiazepine is absolutely necessary, lorazepam is often safer because it is metabolized differently and does not accumulate as readily with age.
People with liver disease, especially cirrhosis, should avoid alprazolam. Phase I benzodiazepines like alprazolam accumulate in hepatic impairment, and benzodiazepines can trigger or worsen hepatic encephalopathy, particularly within three to ten days of starting the medication. Lorazepam or oxazepam are preferred alternatives if a benzodiazepine is essential.
Anyone taking opioid pain medications should not combine them with benzodiazepines. This pairing carries an FDA boxed warning due to risks of profound sedation, respiratory depression, coma, and death. Similarly, alcohol and other sedatives like Z-drugs (Ambien, Lunesta) multiply the sedative effects and should be strictly avoided.
Individuals with a history of substance use disorder face higher risks of benzodiazepine dependence and misuse. National data show that alprazolam is the most frequently implicated medication in emergency department visits for medication harms among young and middle-aged adults, with an estimated 61% of these visits involving alcohol or illicit substances.
Cardiac Safety: Escitalopram’s QT Risk
While alprazolam does not affect heart rhythm, escitalopram can prolong the QT interval on an electrocardiogram in a dose-dependent manner. This effect is driven by drug exposure rather than dose alone, meaning that factors increasing escitalopram blood levels also increase cardiac risk. In older adults, reduced clearance raises peak concentrations; one study found that approximately 20% of patients over 65 exceeded a modeled risk threshold after 10 mg escitalopram, and roughly 60% after 20 mg.
Regulatory agencies recommend dose limits and monitoring for at-risk patients. The UK Medicines and Healthcare products Regulatory Agency advises keeping escitalopram at 10 mg or lower in people over 65 and those with additional risk factors such as congenital long QT syndrome, structural heart disease, or concurrent use of other QT-prolonging medications.
Therapeutic drug monitoring can improve safety. Keeping escitalopram trough levels below 100 nanomolar and timing ECGs near the drug’s peak concentration (about three hours after dosing) helps identify patients at higher risk. A recent study using TDM-guided dosing found that avoiding dose escalation above the therapeutic range reduced adverse drug reactions and prevented significant QTc prolongation.
Safe Use Guidelines for Short-Term Combination Therapy
When combining alprazolam with escitalopram is clinically justified, strict time limits and dose minimization are essential. Use the lowest effective alprazolam dose on an as-needed basis, ideally for no more than one to two weeks. Dispense small quantities without automatic refills and schedule early follow-up to reassess need and side effects.
Counsel patients to avoid driving or operating machinery for several hours after taking alprazolam until they understand their individual response. Alcohol must be avoided entirely, as it substantially increases sedation and respiratory depression risk. Review all other medications, including over-the-counter antihistamines, which can add to the sedative burden.
For older adults or those with liver disease, substitute lorazepam for alprazolam if a benzodiazepine is unavoidable. Start escitalopram at lower doses and titrate conservatively. Consider baseline and follow-up ECGs in patients over 65, those with cardiac disease, or anyone taking other medications that prolong the QT interval.
Establish a clear discontinuation plan from the outset. The 2025 ASAM Joint Guideline on benzodiazepine tapering recommends gradual dose reductions of 5 to 10% at intervals tolerable to the patient, avoiding abrupt discontinuation to prevent withdrawal symptoms like rebound anxiety, insomnia, tremor, and perceptual disturbances.
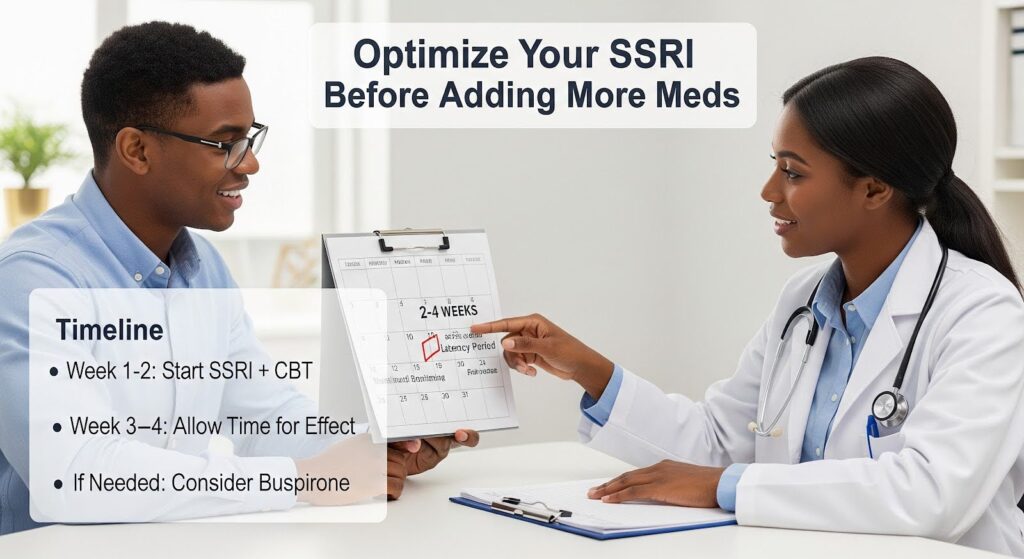
Alternatives to Benzodiazepines During SSRI Initiation
Nonpharmacological strategies should be the first line for managing anxiety during the SSRI latency period. Cognitive behavioral therapy for anxiety and panic, breathing techniques, and sleep hygiene can provide meaningful relief without sedative risks. Some clinicians consider pregabalin as a short-term substitute for benzodiazepines due to its rapid anxiolytic onset, though it also carries CNS depressant effects and requires careful monitoring.
Optimizing the SSRI regimen itself is critical. Ensure adequate dosing and allow sufficient time for therapeutic effect before adding other agents. In selected cases, switching to a different SSRI or adding buspirone (which does not provide acute relief but has no sedative or dependence risk) may be appropriate.
What the Evidence Shows About Co-Prescribing Patterns?
Real-world data reveal that simultaneous benzodiazepine and SSRI initiation is common but not necessarily beneficial. In a large US study of adolescents and young adults newly starting SSRIs for anxiety, 4.3% of adolescents and 16.7% of young adults received a benzodiazepine on the same day, with alprazolam being the most common choice. The median initial supply was 15 days. Importantly, co-initiation was not associated with longer SSRI treatment duration, questioning the routine practice and supporting targeted, time-limited use only when acute distress clearly warrants it.
Pharmacovigilance data underscore the harm potential. Alprazolam ranks as the single most frequently implicated medication in emergency department visits for medication harms among adults aged 15 to 44, with the vast majority involving nontherapeutic use and polydrug exposures. These population-level signals reinforce the need for careful patient selection, robust education about misuse risks, and tight quantity limits.
Monitoring and Patient Education
Effective monitoring starts before the first dose. Screen for substance use history, sleep apnea, fall risk, and all concurrent medications. Correct any electrolyte abnormalities that could amplify cardiac risk. Provide written and verbal counseling about expected side effects, activity restrictions, and the importance of avoiding alcohol and other sedatives.
Encourage patients to keep a simple symptom diary noting the time of doses and any episodes of sleepiness, dizziness, near-falls, or confusion. Early recognition allows timely dose adjustments or discontinuation. Schedule follow-up within one to two weeks to reassess symptoms, adherence, and readiness to begin tapering the benzodiazepine.
For at-risk patients, implement cardiac monitoring. Obtain a baseline ECG and repeat it near escitalopram’s peak concentration after dose increases. If therapeutic drug monitoring is available, use it to guide dosing and keep trough levels below the 100 nanomolar threshold.
Why Does it Matter?
The decision to combine Xanax with Lexapro is not simply a matter of pharmacokinetics. It involves balancing rapid symptom relief against real risks of sedation, falls, cognitive impairment, and in vulnerable groups, cardiac effects and hepatic encephalopathy. The evidence supports short, targeted use with vigilant monitoring and proactive deprescribing, not routine or prolonged coadministration.
Patients deserve transparent information about what they are likely to experience: the first days on this combination often bring noticeable drowsiness and unsteadiness, requiring adjustments to daily routines and strict avoidance of driving and alcohol. Older adults and those with multiple medications face compounded risks that may outweigh benefits, making alternative strategies essential.
Clinical practice should pivot toward individualized care that prioritizes nonpharmacological interventions, optimizes SSRI dosing, and reserves benzodiazepines for the narrowest indications and shortest durations. When the combination is used, explicit plans for tapering and discontinuation must be in place from day one.
If you or a loved one is navigating anxiety or depression treatment and wondering about medication options, professional guidance tailored to your unique situation is essential. Reach out to explore evidence-based treatment that integrates medical expertise with compassionate, individualized care.
