Many people starting treatment for anxiety or panic disorder wonder whether it’s safe to combine Zoloft (sertraline) with clonazepam. A controlled study found no meaningful drug interaction between the two medications at standard doses, yet real-world safety depends heavily on patient age, other medications, and fall risk.
This article explains what the research shows about taking Zoloft and clonazepam together, who faces the highest risks, and how to use these medications safely when both are prescribed.
What Happens When You Combine Zoloft and Clonazepam?
From a drug metabolism standpoint, sertraline and clonazepam do not interfere with each other’s breakdown in the body. A randomized, double-blind study of 13 healthy adults taking clonazepam 1 mg daily with or without sertraline 100 mg daily for 10 days showed no significant changes in clonazepam clearance, blood levels, or half-life. Psychomotor performance tests and sedation ratings remained similar whether participants took clonazepam alone or with sertraline.
Despite this lack of pharmacokinetic interaction, the combination still carries important safety considerations. Both medications affect the central nervous system, and their effects can add up in ways that increase drowsiness, slow reaction times, and raise fall risk, especially in older adults or people taking other sedating drugs.
Why Doctors Sometimes Prescribe Zoloft and Clonazepam Together?
Clinicians may prescribe clonazepam alongside sertraline during the first few weeks of SSRI treatment to manage severe anxiety or panic symptoms while the antidepressant takes effect. Sertraline typically requires four to six weeks to reach full benefit, and clonazepam can provide faster relief during this ramp-up period.
Research on panic disorder found that adding short-term clonazepam to sertraline led to faster symptom improvement at weeks one and three compared with sertraline alone, with similar dropout rates between groups. This supports the clinical utility of brief benzodiazepine bridges when anxiety is disabling and non-drug approaches are insufficient.
The key word is *brief*. International guidelines reviewed through October 2023 consistently recommend limiting benzodiazepine use to two to four weeks when prescribed at all, reserving them for short-term augmentation rather than long-term maintenance.
Who Should Avoid Taking Clonazepam and Zoloft Together?
Older Adults
The American Geriatrics Society Beers Criteria explicitly advises avoiding benzodiazepines in adults 65 and older due to strong evidence linking them to cognitive impairment, delirium, falls, and fractures. Shorter-acting benzodiazepines are not safer than long-acting ones in this population.
Population studies show that co-initiating an SSRI and benzodiazepine in adults 80 and older carries roughly five times higher hip fracture risk, with an estimated 17 people needing to be exposed for one year to cause one additional hip fracture. Adding a benzodiazepine to ongoing SSRI therapy still raises fracture risk, with a number needed to harm of about 32.
People Taking Opioids
The FDA updated benzodiazepine boxed warnings in 2020 to emphasize that combining benzodiazepines with opioids can cause extreme sedation, respiratory depression, coma, and death. If you take prescription opioids for pain, avoid clonazepam unless your prescribers coordinate closely and implement strict safety measures. Even then, the combination should be a last resort.
Individuals with Sleep Apnea
Benzodiazepines can worsen breathing problems during sleep. The STOP-Bang questionnaire (assessing snoring, tiredness, observed apneas, blood pressure, BMI, age, neck size, and gender) screens for obstructive sleep apnea with over 93% sensitivity at scores of three or higher. If you score in this range or have diagnosed sleep apnea, clonazepam may not be safe.
Those on Multiple Sedating Medications
Taking three or more psychotropic medications together increases fall risk significantly. A study of Medicare beneficiaries with chronic pain and anxiety found that combining benzodiazepines, opioids, gabapentinoids, and SSRIs or SNRIs raised fall rates compared with fewer medications. Each additional sedating drug compounds the risk.
Common Side Effects of Zoloft and Clonazepam
| Side Effect | Primary Cause | What to Watch For |
|---|---|---|
| Daytime drowsiness | Clonazepam | Difficulty staying alert, needing naps, trouble concentrating |
| Unsteady gait | Both medications | Feeling wobbly, near-falls, difficulty with balance |
| Nausea or diarrhea | Sertraline | Stomach upset, loose stools (usually improves after 1–2 weeks) |
| Sexual problems | Sertraline | Decreased desire, delayed orgasm |
| Morning grogginess | Clonazepam | Feeling “hungover” or foggy after waking |
| Memory issues | Clonazepam | Trouble recalling recent events, word-finding difficulty |
Sertraline contributes relatively little sedation on its own. Studies in elderly volunteers found minimal psychomotor impairment even at 200 mg daily. The drowsiness and coordination problems people experience with the combination come primarily from clonazepam, though the effects can add up when both drugs are present.
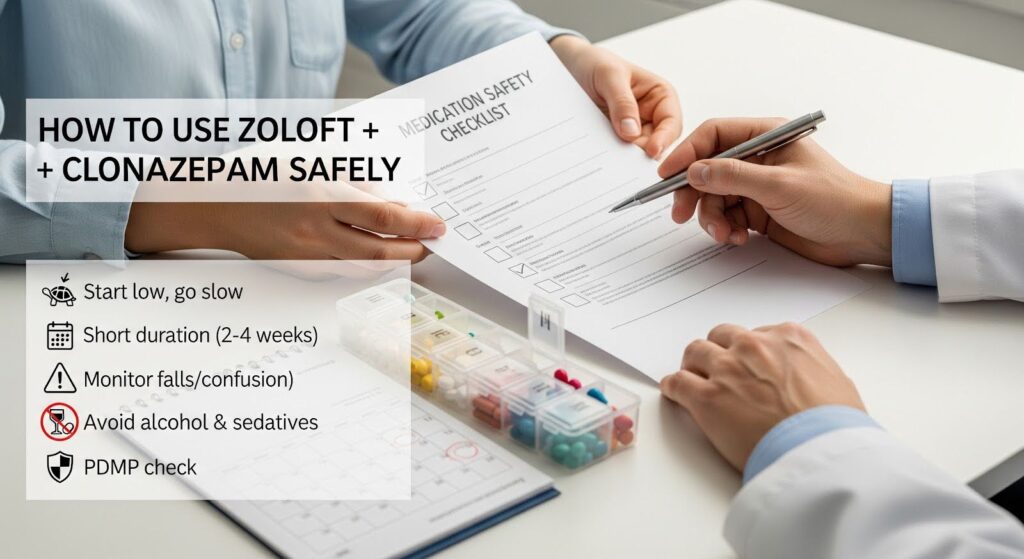
How to Use Zoloft and Clonazepam Safely?
Start Low and Go Slow
Older adults should typically start sertraline at 25 mg daily, increasing by 25 mg every one to two weeks based on response and side effects. For clonazepam, doses as low as 0.125 to 0.25 mg at bedtime may be sufficient for short-term use.
No dose adjustment of clonazepam is needed solely because of sertraline, since the medications don’t interfere with each other’s metabolism. However, lower doses are still appropriate in older adults due to age-related changes in drug clearance and increased sensitivity to sedation.
Plan a Short Duration
Set an explicit stop date for clonazepam before you start, ideally two to four weeks. The highest fall and fracture risk occurs in the first two to four weeks after starting a benzodiazepine, making early monitoring especially important.
Monitor for Falls and Confusion
Check for warning signs weekly during the first month:
- Unsteadiness when standing or walking
- Dizziness or lightheadedness
- Confusion or disorientation
- Excessive sleepiness during the day
- Slowed thinking or difficulty finding words
Simple home safety measures like removing throw rugs, improving lighting, and installing grab bars in bathrooms can reduce fall risk.
Avoid Alcohol and Other Sedatives
Alcohol, over-the-counter sleep aids, sedating antihistamines, and Z-drugs (zolpidem, eszopiclone) all increase central nervous system depression when combined with clonazepam. Avoid these substances entirely while taking both medications.
Use Prescription Drug Monitoring Programs
Your prescribers should check your state’s prescription drug monitoring program (PDMP) before prescribing controlled substances and at regular intervals. These databases track opioid and benzodiazepine prescriptions across providers, helping identify risky combinations.
Tapering Off Clonazepam
Stopping clonazepam abruptly can cause withdrawal symptoms including rebound anxiety, insomnia, irritability, tremors, and in severe cases, seizures. A gradual taper is essential.
Common tapering approaches reduce the dose by 20 to 25% initially, hold for two to four weeks, then continue with 5 to 12.5% reductions every two to four weeks. Older adults and people who have taken clonazepam for months or years may need slower tapers.
Supportive measures during tapering include:
- Continuing sertraline to manage underlying anxiety
- Cognitive behavioral therapy for anxiety or insomnia
- Sleep hygiene improvements
- Regular exercise
- Reassurance that temporary discomfort during tapering is normal
A 2025 joint guideline on benzodiazepine tapering recommends against switching to longer-acting benzodiazepines in older adults due to accumulation risks. Instead, taper the current medication slowly with close monitoring.
When the Combination May Be Appropriate?
Short-term clonazepam added to sertraline can be reasonable in specific situations:
- Severe, disabling panic or anxiety during SSRI initiation when non-drug approaches have failed
- Low fall risk with safety measures in place
- No concurrent opioids or untreated sleep apnea
- Clear plan for tapering within two to four weeks
- Informed consent about risks
Even in these scenarios, the combination should be a bridge, not a destination. The goal is to optimize sertraline and non-medication strategies while phasing out clonazepam as quickly as safely possible.
What the Guidelines Say?
A 2024 international review of 113 clinical practice guidelines found consistent recommendations against using benzodiazepines as first-line treatment for anxiety, insomnia, or depression. When used, duration should be limited to two to four weeks, with increasing emphasis on safe deprescribing.
The U.S. Department of Health and Human Services and SAMHSA issued a 2025 letter urging reduction of chronic benzodiazepine use in older adults, citing substantially higher risks of falls, hip fractures, motor vehicle collisions, delirium, and cognitive impairment. The letter aligns with AGS guidance to avoid benzodiazepines in older adults except in limited circumstances like seizure disorders.
Special Considerations
Cognitive Impairment
Benzodiazepines can worsen confusion and memory problems in people with dementia or mild cognitive impairment. Avoid clonazepam in these populations when possible, prioritizing non-sedating treatments.
Driving Safety
Both medications can impair reaction time and coordination. Avoid driving when starting either medication, after dose increases, or whenever you feel drowsy or unsteady. The risk is highest in the first few weeks.
Pregnancy and Breastfeeding
Discuss risks and benefits with your healthcare provider if you are pregnant, planning pregnancy, or breastfeeding. Both medications cross the placenta and enter breast milk.

Alternatives to Consider
Before adding clonazepam to sertraline, consider:
- Optimizing sertraline dose and allowing adequate time for response (six to eight weeks)
- Cognitive behavioral therapy for anxiety or panic disorder
- Mindfulness-based stress reduction
- Exercise and sleep hygiene improvements
- Buspirone as a non-sedating anxiolytic option
- Hydroxyzine for short-term anxiety relief (though it also causes sedation)
The Bottom Line
You can take Zoloft and clonazepam together without worrying about drug interactions that change how your body processes either medication. The real safety concerns center on additive sedation, fall risk, and the potential for benzodiazepine dependence, especially in older adults.
If your doctor prescribes both medications, ask about the plan for stopping clonazepam, what warning signs to watch for, and how to reduce fall risk. Most people should use clonazepam for no more than two to four weeks while sertraline takes effect.
Older adults, people taking opioids, and those with sleep apnea or multiple sedating medications face substantially higher risks and should generally avoid the combination unless no safer alternatives exist.
If you’re struggling with anxiety or panic symptoms and wondering whether medication is right for you, reach out for professional guidance. The Summit Wellness Group offers dual diagnosis treatment that addresses both mental health and substance use concerns with individualized, evidence-based care in a supportive environment.
