Many people with panic disorder or severe anxiety wonder whether combining medications will help them feel better faster.
Taking Zoloft and Klonopin together can accelerate early symptom relief in panic disorder, with one trial showing 41% of patients responding within the first week compared to just 4% on Zoloft alone.
This article explains when this combination is appropriate, what side effects to expect, and how to use both medications safely.
What Are Zoloft and Klonopin?
Zoloft (sertraline) is a selective serotonin reuptake inhibitor (SSRI) approved for major depression, panic disorder, social anxiety disorder, obsessive-compulsive disorder, and PTSD. It works by increasing serotonin levels in the brain, but this effect takes several weeks to fully develop. Common early side effects include nausea, dizziness, insomnia or drowsiness, and headaches.
Klonopin (clonazepam) is a long-acting benzodiazepine that enhances GABA activity in the brain, producing rapid anxiety relief. It is FDA-approved for seizure disorders and panic disorder. While effective for acute anxiety, clonazepam carries risks of sedation, cognitive slowing, tolerance, dependence, and withdrawal symptoms when stopped abruptly.
Can You Take Zoloft and Klonopin Together?
Yes, but only under specific conditions and for a limited time. The combination is most appropriate as a short-term “bridge” strategy in moderate to severe panic disorder, where clonazepam provides immediate relief while waiting for Zoloft to take effect.
A randomized controlled trial tested this approach in 50 adults with panic disorder. All participants received sertraline titrated to 100 mg daily. Half also received clonazepam 0.5 mg three times daily for four weeks, followed by a three-week taper.
The clonazepam group showed significantly higher response rates at week one (41% versus 4%) and week three (63% versus 32%). However, by the end of treatment, response rates were similar between groups, confirming that clonazepam accelerates improvement without providing long-term advantages.
Common Side Effects When Taking Zoloft and Klonopin Together
The primary concern when combining these medications is additive sedation and psychomotor impairment. Understanding the side effect profile of each drug helps you anticipate what to watch for.
Drowsiness and Somnolence
Somnolence is the principal adverse effect of clonazepam in panic disorder trials. Zoloft can also cause drowsiness, especially early in treatment. When taken together, sedation may be more pronounced, affecting your ability to drive, operate machinery, or perform tasks requiring sustained attention.
Dizziness and Balance Issues
Both medications can cause dizziness. Zoloft-related dizziness is common during the first weeks of treatment and after abrupt discontinuation. Combined with clonazepam, this effect increases fall risk, particularly in older adults.
Cognitive and Attention Problems
Patients report concentration difficulties on both medications. Clonazepam can cause dose-related cognitive slowing, while Zoloft users sometimes describe a “lack of concentration.” Together, these effects may impair work performance, learning, and memory.
Sleep Disturbances
Zoloft can cause either insomnia or somnolence. Clonazepam typically improves sleep but carries a risk of rebound insomnia during withdrawal. The combination may initially help with SSRI-induced insomnia, but careful tapering is essential to avoid sleep disruption later.
Other Common Effects
- Gastrointestinal upset and headache (primarily from Zoloft)
- Early anxiety or jitteriness from Zoloft, which clonazepam may offset
- Sexual dysfunction (SSRI class effect)
Interaction Risk: Pharmacology and Safety
No Significant Pharmacokinetic Interaction
A controlled study in healthy volunteers found no clinically meaningful pharmacokinetic interaction between clonazepam and sertraline at therapeutic doses. Clonazepam clearance and half-life remained stable when combined with sertraline, and psychomotor impairment measures showed less than 10% change from drug-free baselines. This suggests the combination risk is primarily pharmacodynamic (additive CNS depression) rather than metabolic.
Additive CNS Depression
The main interaction is additive sedation and psychomotor slowing. This pharmacodynamic effect increases risks of falls, motor vehicle accidents, and cognitive dysfunction, especially in vulnerable populations.
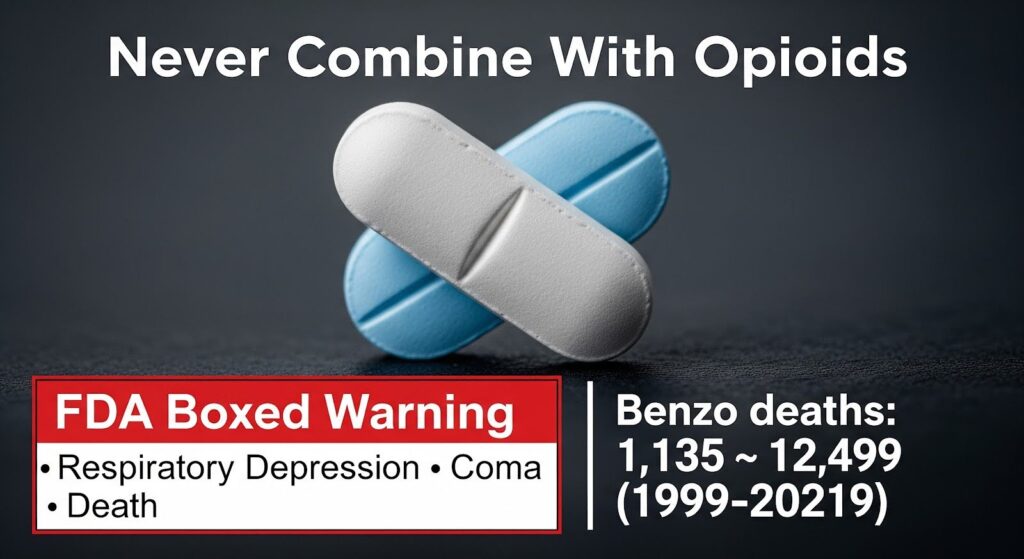
Critical Contraindication: Opioid Co-Use
The FDA issued a boxed warning against combining benzodiazepines with opioids due to synergistic respiratory depression, which can result in profound sedation, coma, and death. Benzodiazepine-related overdose deaths in the U.S. rose from 1,135 in 1999 to 12,499 in 2021, with opioid co-exposure a major contributor. If you take any opioid medication, avoid benzodiazepines entirely.
Driving and Psychomotor Impairment
Benzodiazepines consistently impair driving performance in standardized on-road tests. Studies using the standard deviation of lateral position (SDLP) measure show that benzodiazepines like lorazepam produce clinically significant impairment, often exceeding the threshold equivalent to a blood alcohol concentration of 0.05%.
Clonazepam’s long half-life raises concerns about residual next-day impairment, particularly during dose initiation or increases. Do not drive or operate heavy machinery during the first weeks of combination therapy or after any dose change. Resume these activities only when you feel fully alert and free of sedation.
Who Should Avoid This Combination?
Older Adults
The American Geriatrics Society Beers Criteria strongly recommend avoiding benzodiazepines in adults 65 and older due to increased sensitivity and risks of cognitive impairment, delirium, falls, fractures, and motor vehicle crashes. Shorter-acting benzodiazepines are not safer. If you are an older adult, discuss non-benzodiazepine alternatives with your doctor.
People Taking Opioids or With Opioid Use Disorder
Avoid benzodiazepines if you take any opioid medication, including short courses for acute pain. In opioid use disorder treatment, benzodiazepines are associated with elevated poisoning risk. Non-GABAergic options like cognitive behavioral therapy, trazodone, or melatonin receptor agonists are preferred for insomnia and anxiety in this population.
Individuals With High Fall Risk or Cognitive Impairment
Benzodiazepines worsen outcomes in people with cognitive impairment and increase fall-related injuries. If you have dementia, balance problems, or a history of falls, avoid this combination.
People in Safety-Sensitive Occupations
If your job involves driving, operating machinery, or other safety-critical tasks, the sedation and psychomotor impairment from this combination pose unacceptable risks. Consider alternative treatments or implement strict no-driving policies during treatment initiation.
Pregnancy and Hepatic Impairment
Zoloft exposure increases in hepatic impairment; doses should be halved in mild impairment and avoided in moderate to severe disease. The oral solution contains 12% alcohol and is not recommended during pregnancy. Third-trimester SSRI exposure may increase neonatal adaptation issues. Discuss risks and benefits with your healthcare provider if you are pregnant or have liver disease.
When Is the Combination Appropriate?
Moderate to Severe Panic Disorder
The clearest evidence-based use is early stabilization in panic disorder. The trial-tested regimen involves:
- Zoloft: Start 25 mg daily for one week, increase to 50 mg at week two, then 100 mg at week three
- Klonopin: 0.5 mg three times daily (total 1.5 mg/day) for four weeks
- Taper: Reduce clonazepam over three weeks (for example, decrease by 0.5 mg weekly)
- Duration: Seven weeks total of benzodiazepine use (four weeks full dose plus three-week taper)
This approach is appropriate only if you are not an older adult, not taking opioids, do not have opioid use disorder, have low fall and cognitive risk, and can adhere to a structured taper plan.
Social Anxiety Disorder After SSRI Nonresponse
A trial in social anxiety disorder found that adding clonazepam (up to 3 mg daily) after ten weeks of sertraline nonresponse improved symptom severity and disability scores compared to continuing sertraline alone. However, remission rates did not differ significantly. This suggests clonazepam augmentation may help some nonresponders, but should remain time-limited with a clear taper plan and specialist guidance.
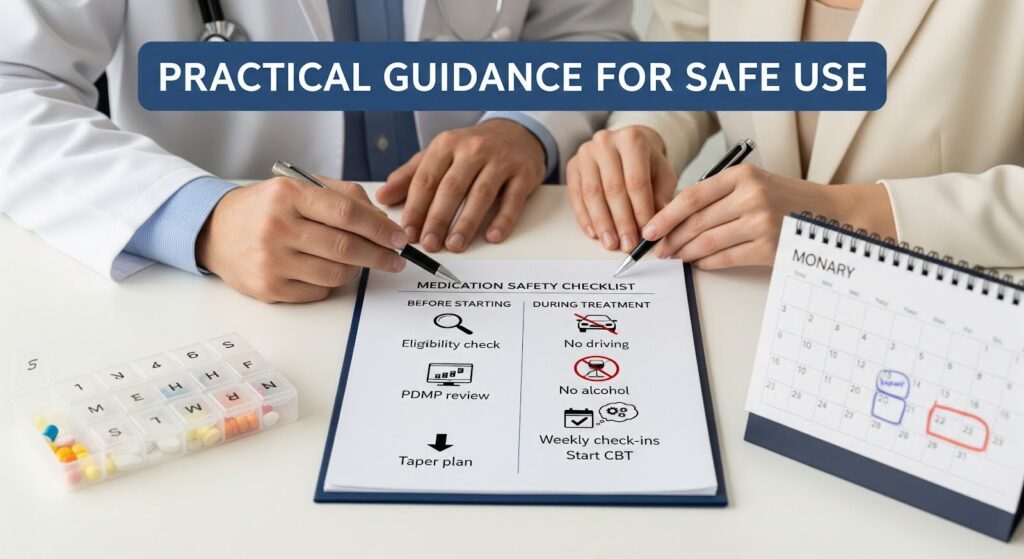
Practical Guidance for Safe Use
Before Starting
- Confirm the indication is appropriate (panic disorder requiring rapid stabilization)
- Check for exclusions: age 65 or older, opioid use, opioid use disorder, high fall or cognitive risk, moderate to severe liver disease
- Complete a prescription drug monitoring program (PDMP) check to verify no other benzodiazepines or opioids
- Discuss dependence and withdrawal risks, sedation, driving restrictions, and the exact taper plan
- Document the treatment plan and exit strategy
During Treatment
- Avoid driving and operating machinery during the first weeks and after dose changes
- Do not use alcohol or sedating over-the-counter antihistamines (products labeled “PM”)
- Schedule weekly check-ins during the first month to assess sedation, falls, panic frequency, and adherence
- Transition to biweekly monitoring during the taper phase
- Start cognitive behavioral therapy (CBT) early to improve long-term outcomes and support benzodiazepine discontinuation
Tapering Clonazepam
Follow the planned taper schedule. General deprescribing guidance suggests reducing the dose by approximately 25% every two weeks, with slower reductions (around 12.5%) near the end for patients on longer courses or higher doses. Monitor for withdrawal symptoms such as rebound anxiety, insomnia, or autonomic symptoms. If troublesome symptoms emerge, pause at the current dose and resume tapering at a slower rate after stabilization.
Continuing Zoloft
Maintain Zoloft for relapse prevention in panic disorder. Adjust the dose gradually based on response and side effects. Avoid abrupt discontinuation, which can cause dizziness and insomnia that impair daily functioning.
Alternatives to Reduce Benzodiazepine Exposure
- Cognitive behavioral therapy (CBT): First-line treatment for panic disorder with durable benefits; integrating CBT during benzodiazepine taper nearly doubles successful discontinuation rates
- CBT for insomnia (CBT-I): Preferred over benzodiazepines for sleep problems
- Non-GABAergic medications: Trazodone, melatonin receptor agonists, or hydroxyzine for insomnia or anxiety in patients with opioid use disorder
- SSRI or SNRI optimization: Adequate dose and duration trials before considering augmentation
Monitoring Checklist
Track these outcomes during combination therapy:
- Daytime sleepiness and sedation
- Dizziness and falls or near-falls
- Concentration and attention problems
- Driving near-misses or safety concerns
- Respiratory suppression (especially if any opioid exposure)
- Insomnia changes during taper
- Anxiety relapse or panic frequency
Evidence-Based Recommendations
Based on randomized controlled trials, network meta-analyses, and contemporary guidelines from NICE and the American Geriatrics Society, the following recommendations apply:
Appropriate use: Co-prescribe Zoloft and Klonopin for a short, pre-defined period (up to seven weeks) in moderate to severe panic disorder to accelerate stabilization, using the trial-tested dosing regimen, provided the patient is not on opioids, is not an older adult, does not have high fall or cognitive risk or opioid use disorder, and can adhere to a structured taper with CBT integration.
Avoid in: Older adults, anyone taking opioids or with opioid use disorder, individuals with high fall or cognitive risk, people in safety-sensitive occupations without strict activity restrictions, and for primary insomnia.
Always include: Informed consent about dependence and withdrawal, PDMP checks, limited dispensing (weekly quantities initially), no early refills, explicit driving and machinery restrictions, early CBT initiation, and a documented individualized taper plan with close monitoring.
Why Does it Matter?
Panic disorder and severe anxiety can be disabling. The combination of Zoloft and Klonopin offers a scientifically supported way to reduce suffering in the critical early weeks of treatment. However, the benefits are time-limited, and the risks, especially sedation, dependence, falls in older adults, and respiratory depression with opioids, are real and sometimes severe.
Using this combination safely requires deliberate structure: the right patient, the right indication, the right dose and duration, explicit safety counseling, and a commitment to tapering and transitioning to long-term strategies like SSRI maintenance and psychotherapy. When these conditions are met, the combination can be an appropriate bridge to stability. When they are not, the risks outweigh the benefits, and safer alternatives should be pursued.
If you or someone you care about is struggling with panic disorder or anxiety and considering medication options, reach out to a qualified treatment provider who can assess your individual needs and design a comprehensive, evidence-based plan. Contact our team to discuss personalized treatment options that prioritize both rapid relief and long-term safety.
