Many people starting treatment for anxiety or panic disorder wonder whether their doctor will prescribe both Lexapro and Klonopin at the same time.
The short answer is yes, doctors sometimes prescribe these medications together for a brief period, typically two to four weeks, when someone needs rapid symptom relief while waiting for the antidepressant to take full effect.
For example, a person experiencing frequent panic attacks may receive clonazepam to quickly reduce attack frequency while escitalopram builds therapeutic levels over several weeks.
This article explains when combined therapy makes sense, what risks you should know about, and how to use both medications safely under medical supervision.
Understanding Lexapro and Klonopin
Lexapro (escitalopram) is a selective serotonin reuptake inhibitor that treats depression and generalized anxiety disorder by gradually increasing serotonin levels in the brain. The medication typically requires several weeks to reach full effectiveness, and during the initial phase some people experience temporary increases in anxiety or insomnia.
Klonopin (clonazepam) belongs to the benzodiazepine class and works by enhancing GABA activity in the brain, producing rapid calming effects within hours. Doctors prescribe it for panic disorder and certain seizure conditions. Unlike Lexapro, clonazepam provides immediate relief but carries significant risks when used long term, including physical dependence in nearly all patients who take it regularly for more than one month.
When Doctors Prescribe Both Medications?
Research shows that combining an SSRI with a benzodiazepine at treatment start can help in specific situations. Small randomized trials found that adding clonazepam to an SSRI like sertraline or paroxetine accelerated early symptom control in the first five weeks of panic disorder treatment, though outcomes at 12 weeks were similar to SSRI alone.
Doctors most commonly recommend using Lexapro and Klonopin together when:
- Starting treatment for acute panic disorder with frequent, severe attacks
- Managing significant anxiety or insomnia that worsens when beginning Lexapro
- Bridging the gap until the antidepressant reaches therapeutic effect
A study of commercial insurance claims found that among young people starting SSRIs for anxiety, 4.3% of adolescents and 16.7% of young adults received a benzodiazepine prescription at the same time. Those who received both medications had fewer recent psychotherapy visits and more emergency department encounters, suggesting the combination often addresses higher acute severity or limited access to counseling.
Important Safety Risks of Combined Use
Central Nervous System Depression
Both medications can cause drowsiness, but clonazepam produces more pronounced sedation that worsens when combined with other substances. The FDA requires a boxed warning on all benzodiazepines about risks of abuse, misuse, addiction, physical dependence, and withdrawal.
Combining clonazepam with opioid pain medications creates profound sedation, respiratory depression, coma, and death risk. National survey data from 2011 to 2020 showed that 14% of adults using either opioids or benzodiazepines reported taking both within 30 days, with higher rates among people with sleep problems, arthritis, or depression symptoms.
Physical Dependence and Withdrawal
The 2025 Joint Clinical Practice Guideline on Benzodiazepine Tapering emphasizes that regular benzodiazepine use for more than one month leads to physical dependence in nearly all patients. This differs from addiction but means your body adapts to the medication and experiences withdrawal symptoms if you stop abruptly. Symptoms can include anxiety rebound, insomnia, tremor, and in severe cases, seizures.
Because of this risk, doctors should establish a written taper plan from day one when prescribing clonazepam, even for short-term use.
Cardiac Considerations with Lexapro
Escitalopram can cause dose-dependent QTc prolongation, a change in heart electrical activity that increases risk of dangerous heart rhythms. Risk increases with age, existing heart disease, low potassium or magnesium levels, liver problems, and medications that also prolong QTc intervals. While serious outcomes remain uncommon, doctors should assess cardiac risk factors before prescribing higher escitalopram doses or combining with other QT-prolonging drugs.
Serotonin Syndrome Risk with Other Medications
While clonazepam does not cause serotonin syndrome, people taking Lexapro must avoid certain over-the-counter cough medicines. Case reports with confirmed blood levels document serotonin syndrome when dextromethorphan was combined with therapeutic SSRI doses. Additional cases occurred after overdoses of OTC cough products containing dextromethorphan. Always check with your pharmacist before using cold or cough remedies while taking escitalopram.
Special Populations Requiring Extra Caution
Older Adults
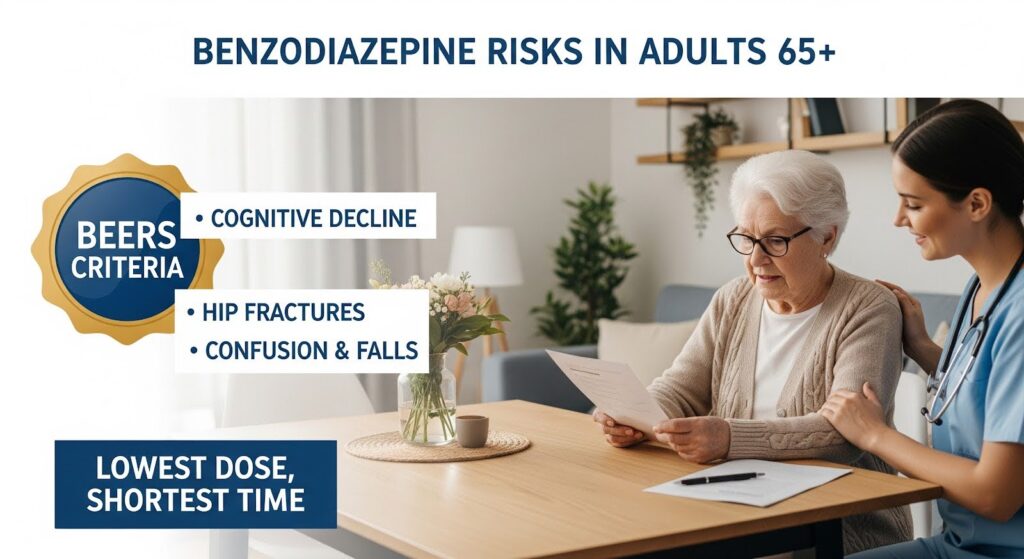
People 65 and older face heightened risks from benzodiazepines, including falls, hip fractures, confusion, and cognitive decline. The Beers Criteria for potentially inappropriate medication use in older adults flags benzodiazepines as medications to avoid when possible. If use becomes necessary, doctors should prescribe the lowest dose for the shortest time with fall prevention strategies and frequent medication reviews.
People with Respiratory Conditions
Clonazepam can worsen breathing problems in people with chronic obstructive pulmonary disease or obstructive sleep apnea by depressing respiratory drive. Doctors should avoid prescribing it in these situations or use extreme caution with close monitoring for daytime sleepiness and breathing difficulties.
Pregnancy and Breastfeeding
Escitalopram is generally compatible with breastfeeding, with low infant exposure and rare reports of temporary infant sleepiness. Research shows that starting or restarting antidepressants postpartum associates with lower breastfeeding rates at six months. Benzodiazepine use during breastfeeding requires individualized assessment with pediatric input to monitor infants for sedation and feeding problems.
Concurrent Substance Use
People who drink alcohol heavily or use other sedatives should not receive benzodiazepines due to dangerous interactions. Alcohol combined with these medications worsens sedation, impairs coordination, and increases overdose risk. The National Institute on Alcohol Abuse and Alcoholism explicitly warns against mixing alcohol with psychotropic medications.
How to Use Both Medications Safely?
Duration and Dosing Strategy
Current guidance recommends limiting benzodiazepine use to two to four weeks when treating anxiety, except in rare circumstances. Doctors should:
- Start with the lowest effective clonazepam dose
- Set a specific stop date before writing the first prescription
- Begin escitalopram at a low dose (often 5 mg daily) and increase gradually
- Schedule follow-up within one to two weeks to assess response and side effects
Timing Considerations
If Lexapro causes insomnia, taking it in the morning may help. When it causes sleepiness, bedtime dosing works better. Doctors often recommend taking clonazepam at bedtime to reduce daytime drowsiness, though its long duration of action can still cause next-day grogginess.
Essential Patient Counseling
Before starting combined therapy, your doctor should discuss:
- Avoiding alcohol completely while taking both medications
- Not driving or operating machinery until you know how the medications affect you
- Staying away from dextromethorphan-containing cough products
- Understanding that clonazepam is a short-term bridge, not a long-term solution
- Following the taper schedule carefully when it’s time to stop
Monitoring Requirements
Your treatment team should:
- See you within one to two weeks after starting to check symptom response and side effects
- Review all other medications, especially opioids, sedating antihistamines, and other psychotropics
- Consider baseline ECG and electrolyte tests if you have cardiac risk factors
- Check prescription drug monitoring databases when appropriate
- Begin tapering clonazepam as planned, typically after two to four weeks
The Tapering Process
When the time comes to stop clonazepam, your doctor will create an individualized taper schedule based on how long you’ve taken it, your dose, other health conditions, and your preferences. Typical approaches reduce the total daily dose by 5% to 25% every one to two weeks, with pauses to let your body adjust.
People who have taken higher doses for longer periods need slower tapers. Older adults, those with other substance use concerns, or anyone experiencing difficult withdrawal symptoms should work with specialists who can provide patient-centered, flexible tapering with appropriate support.
Never stop clonazepam abruptly without medical guidance, as sudden discontinuation can trigger seizures and severe withdrawal symptoms.
Comparison of Key Features
| Feature | Lexapro (Escitalopram) | Klonopin (Clonazepam) |
|---|---|---|
| Medication class | SSRI antidepressant | Benzodiazepine |
| Speed of effect | 2–4 weeks for full benefit | Hours to days |
| Primary use in combination | Long-term anxiety/depression control | Short-term symptom bridge |
| Dependence risk | Low | High after >1 month |
| Main safety concerns | QTc prolongation, serotonin syndrome with certain drugs | CNS/respiratory depression, falls, dependence |
| Typical duration | Months to years | Days to 2–4 weeks when combined |
| Withdrawal risk | Discontinuation syndrome if stopped abruptly | Severe withdrawal, seizure risk |
When Combined Therapy Should Be Avoided?
Doctors should not prescribe Lexapro and Klonopin together when:
- You currently take opioid pain medications
- You have significant lung disease like COPD or sleep apnea
- You are 65 or older with fall risk or cognitive concerns
- You have active alcohol or substance use problems
- You have access to effective psychotherapy like cognitive behavioral therapy
In these situations, the risks outweigh potential benefits. Alternative approaches include starting Lexapro alone with close monitoring, using non-benzodiazepine sleep aids if needed, or prioritizing evidence-based psychotherapy while medications take effect.

Alternative Strategies
Research shows that adding the sleep medication eszopiclone to escitalopram improved sleep and daytime function in generalized anxiety disorder, with modest improvements in overall anxiety ratings. This demonstrates that non-benzodiazepine options can sometimes substitute for benzodiazepine bridges when insomnia dominates the clinical picture.
Cognitive behavioral therapy for anxiety and panic disorder provides durable benefits without medication risks. Starting CBT at the same time as Lexapro, rather than adding Klonopin, represents the safest long-term approach for most people.
Why This Matters for Your Treatment?
Understanding the narrow role of combined Lexapro and Klonopin therapy helps you make informed decisions with your doctor. The evidence supports short-term use in specific situations, primarily acute panic disorder or severe SSRI activation, but not routine or prolonged co-prescribing.
The 2025 consensus guidance on benzodiazepine tapering reflects growing recognition that these medications carry serious risks that accumulate with time. Physical dependence develops in nearly all regular users after one month, cognitive effects worsen in older adults, and dangerous interactions with opioids and alcohol remain common.
When your doctor recommends both medications, ask about the specific indication, expected duration, taper plan, and alternatives. If you’re already taking both beyond the recommended two to four weeks, request a medication review to discuss safe tapering strategies and whether continuing clonazepam remains appropriate.
The goal is not to avoid helpful treatment but to use powerful medications wisely, getting rapid relief when you need it most while protecting your long-term health and function.
If you or someone you care about is navigating anxiety treatment and concerned about medication safety, professional guidance makes all the difference. Reach out to explore evidence-based treatment options that address both immediate symptoms and lasting recovery.
