If you live with obsessive-compulsive disorder, you know how overwhelming intrusive thoughts and compulsive rituals can be. Some doctors prescribe clonazepam, sold as Klonopin, to ease the anxiety that comes with OCD. But does this benzodiazepine actually help the core symptoms of obsessions and compulsions?
Research shows it generally does not. While Klonopin may calm short-term anxiety, controlled trials found no meaningful improvement in OCD symptoms themselves, and the medication carries serious risks including dependence, sedation, and falls.
This article explains what the evidence says about Klonopin for OCD, when it might be considered, and which treatments actually work.
What is Klonopin and How Does it Work?
Clonazepam is a high-potency benzodiazepine that enhances GABA-A receptor activity in the brain, producing calming, sedative, and muscle-relaxant effects. The FDA approved it for seizure disorders and adult panic disorder, but not for OCD.
Its long half-life means it stays in your system longer than some other benzodiazepines, which can smooth out anxiety but also increases the risk of accumulation and side effects with regular use.
The drug works quickly to dampen anxiety and panic, which is why clinicians sometimes consider it for the severe distress that can accompany OCD. However, OCD’s core pathology involves intrusive thoughts and repetitive behaviors driven by maladaptive habit circuits and error-monitoring hyperactivity in the brain.
These respond to serotonergic medications like SSRIs and to exposure and response prevention therapy, not to the general anxiety suppression that benzodiazepines provide.
Does Klonopin Help OCD Symptoms?
The short answer is no. Randomized controlled trials specifically testing clonazepam in OCD have consistently shown it does not improve obsessions or compulsions. In a 10-week double-blind study, 25 adults with OCD received either clonazepam or placebo.
Researchers measured outcomes using the Yale-Brown Obsessive-Compulsive Scale, the gold standard for tracking OCD severity, along with anxiety and depression scales. Clonazepam was not superior to placebo on any measure. Only one person on clonazepam and two on placebo met responder criteria, leading the authors to conclude that clonazepam is not effective as monotherapy for OCD.
A separate trial tested whether adding clonazepam to sertraline, an SSRI, would boost results in people who had not responded to the SSRI alone. This small study of 37 participants found no significant difference in OCD outcomes between the combination and sertraline plus placebo.
The trial was underpowered to detect small effects, so it cannot definitively rule out a modest benefit, but it certainly does not support routine use of clonazepam as an augmentation strategy.
Klonopin Works for Panic, Not OCD
The contrast with panic disorder is striking. Multiple rigorous trials show clonazepam reduces panic attacks and anxiety in people with panic disorder. In one six-week study, 61.5% of participants on clonazepam became panic-free compared to just 11.1% on placebo.
Similarly, when added to sertraline in people with social anxiety disorder who had not fully responded, clonazepam improved social anxiety symptoms and disability more than placebo.
These findings underscore an important point: benzodiazepines like Klonopin target state anxiety and panic, not the obsessive-compulsive mechanisms that drive OCD. You might feel calmer on Klonopin, but your intrusive thoughts and compulsions are unlikely to improve in a meaningful or lasting way.
What Do Clinical Guidelines Say About Klonopin and OCD?
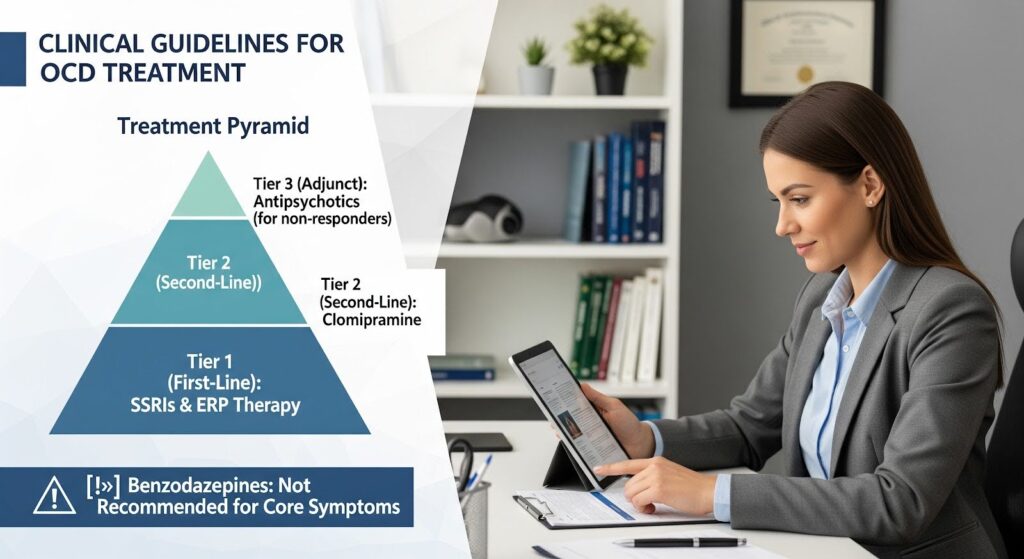
Major treatment guidelines do not recommend benzodiazepines for OCD. The National Institute for Health and Care Excellence and international psychopharmacology reviews identify SSRIs and exposure and response prevention therapy as first-line treatments.
If an SSRI does not work well enough after 12 weeks, guidelines suggest adding ERP or switching to another SSRI or clomipramine, a tricyclic antidepressant with strong anti-obsessional effects.
A 2020 review of OCD pharmacotherapy states that initial treatment should not include anxiolytics, with one narrow exception: cautious, short-term use to manage activation or agitation that sometimes occurs when starting an SSRI. Even in that scenario, the goal is not to treat OCD itself but to help you tolerate the early side effects of the medication that will actually address your symptoms.
The World Federation of Societies of Biological Psychiatry guidelines recognize benzodiazepines may have a role in treatment-resistant anxiety disorders, but OCD is not singled out as a benzodiazepine-responsive condition. The pharmacologic core of OCD treatment remains serotonergic.
Serious Risks of Klonopin You Should Know
Dependence and Withdrawal
Klonopin is a Schedule IV controlled substance with significant potential for dependence. The FDA added a boxed warning in 2020 highlighting risks of abuse, addiction, physical dependence, and withdrawal, which can be severe and prolonged. Stopping abruptly after regular use can trigger dangerous withdrawal symptoms including seizures, so any discontinuation must be gradual and supervised.
A 2025 joint clinical practice guideline on benzodiazepine tapering emphasizes individualized, slow dose reductions with pauses to manage symptoms, often paired with behavioral support such as cognitive behavioral therapy. Withdrawal can be protracted in some cases, making it critical to plan an exit strategy before starting.
Falls and Fractures in Older Adults
Benzodiazepines significantly increase the risk of falls and hip fractures, especially in older adults. A 2022 cohort study of nearly 380,000 older adults newly prescribed a benzodiazepine found that fall injury risk was concentrated in the first 10 days after starting the medication. Short initial prescriptions of less than 14 days were associated with 37% higher fall injury risk than 14 to 30 day fills, and taking an antipsychotic or opioid at the same time increased risk further.
These findings are especially concerning for people with OCD, who may be on multiple medications or have comorbid conditions. The immediate post-initiation hazard means even brief use carries real danger, particularly if you are older, have balance or mobility issues, or take other central nervous system depressants.
Cognitive and Psychomotor Impairment
Klonopin commonly causes sedation, slowed thinking, reduced coordination, and impaired attention. You may feel foggy, have trouble concentrating, or experience slowed reaction times. These effects can interfere with driving, work, and daily functioning. In older adults, cognitive impairment from benzodiazepines is well documented and contributes to the recommendation to avoid them in this population per the American Geriatrics Society Beers Criteria.
Risks During Pregnancy
Benzodiazepines cross the placenta and can cause neonatal sedation and withdrawal syndromes, sometimes called floppy infant syndrome. Chronic use during pregnancy is generally avoided, and if a benzodiazepine is deemed necessary, careful perinatal monitoring is required. For OCD during pregnancy, safer options include exposure therapy and SSRIs with established safety profiles.
What Actually Works for OCD?
Exposure and Response Prevention Therapy
ERP is the most effective psychological treatment for OCD. It involves gradually confronting feared situations or thoughts while resisting the urge to perform compulsions. This process helps your brain learn that the feared outcome does not occur and that you can tolerate the distress without rituals.
Research consistently shows ERP reduces OCD symptoms, and newer approaches using inhibitory learning principles have refined the therapy to reduce relapse. Combining ERP with SSRIs improves outcomes more than medication alone, underscoring ERP’s central role.
Access to trained ERP therapists can be limited, but telehealth, group formats, and internet-based programs are expanding availability. Virtual reality exposure and computer-assisted self-help are emerging tools that can supplement traditional therapy.
SSRIs and Clomipramine
Selective serotonin reuptake inhibitors such as fluoxetine, fluvoxamine, paroxetine, sertraline, and citalopram are first-line medications for OCD. They work by increasing serotonin activity in the brain, which helps reduce obsessions and compulsions over weeks to months. Doses for OCD are often higher than for depression, and treatment should continue for at least 12 months after remission to prevent relapse.
If one SSRI does not work well enough after an adequate trial, switching to another SSRI or to clomipramine is recommended. Clomipramine is a tricyclic antidepressant with strong anti-obsessional effects, though it has more side effects than SSRIs and requires careful monitoring.
For treatment-resistant OCD, evidence supports augmenting an SSRI with low-dose atypical antipsychotics such as risperidone, not with benzodiazepines. Advanced interventions like repetitive transcranial magnetic stimulation or deep brain stimulation may be considered in specialized centers for severe, refractory cases.
When Might Klonopin Be Considered for OCD?
Given the lack of efficacy for core OCD symptoms and the serious safety risks, Klonopin should not be part of routine OCD treatment. A very limited, time-bound role may exist in one narrow scenario: severe, disabling panic or anxiety that acutely prevents you from starting ERP or tolerating early SSRI side effects.
If a clinician considers Klonopin in this context, the following safeguards are essential:
- Use the lowest effective dose for the shortest feasible period.
- Start ERP and an SSRI at the same time, with explicit exit criteria such as beginning a taper once ERP is underway and the SSRI reaches a therapeutic dose.
- Avoid use in older adults, pregnant or breastfeeding individuals, people with a history of substance use disorders, or anyone at high risk for falls.
- Do not combine with opioids, antipsychotics, or other central nervous system depressants.
- Document a taper plan before starting.
This approach acknowledges Klonopin’s robust anxiolytic effects while respecting the absence of anti-obsessional efficacy and the meaningful harms. The therapeutic target is distress tolerance to enable ERP and SSRI treatment, not relief of obsessions or compulsions.

What to Do If You Are Already Taking Klonopin for OCD?
If you are currently taking Klonopin for OCD, talk with your doctor about a gradual taper paired with evidence-based OCD treatment. Stopping benzodiazepines abruptly is dangerous, so any discontinuation must be slow and supervised.
A typical taper might start with a 10 to 25% reduction in your total daily dose, held for two to four weeks, followed by smaller reductions of 5 to 12.5% at similar intervals. The pace should be individualized based on how you respond, with flexibility to pause or adjust if withdrawal symptoms emerge. Combining the taper with ERP-based cognitive behavioral therapy improves outcomes and helps you manage anxiety without relying on medication.
Patient-directed interventions such as educational materials and structured self-management programs can support deprescribing. Studies show these tools help 14 to 72% of older adults successfully stop benzodiazepines, with comparable success in those with mild cognitive impairment.
Summary: Klonopin and OCD Do Not Mix
| Question | Answer |
|---|---|
| Does Klonopin help core OCD symptoms? | No. Controlled trials show no improvement in obsessions or compulsions. |
| Does Klonopin help anxiety or panic? | Yes, in the short term, but this does not translate to OCD symptom relief. |
| What are the main risks? | Dependence, withdrawal, falls (especially in older adults), sedation, cognitive impairment. |
| When might it be used? | Rarely, as a short-term bridge for severe panic preventing ERP or SSRI initiation, with strict safeguards. |
| What works for OCD? | Exposure and response prevention therapy and SSRIs or clomipramine. |
Moving Forward With Effective OCD Treatment
The evidence is clear: Klonopin does not treat the core symptoms of OCD. While it may dampen anxiety in the short term, it does not reduce obsessions or compulsions in a meaningful or lasting way, and it carries serious risks including dependence, falls, and cognitive impairment.
The responsible, patient-centered approach is to prioritize exposure and response prevention therapy and optimize SSRI or clomipramine treatment, reserving Klonopin only for rare, carefully managed situations with a pre-planned taper.
If you or a loved one is struggling with OCD and co-occurring anxiety or substance use, comprehensive care that addresses both conditions is essential. Reach out to explore Summit’s dual diagnosis treatment that integrates evidence-based therapies with the support you need for lasting recovery.
