Many people taking Klonopin for anxiety or panic disorder wonder whether the medication might worsen their mood. Clonazepam, sold as Klonopin, can contribute to depressive symptoms in some patients, especially with prolonged use or during withdrawal.
Evidence from pharmacovigilance systems and clinical studies shows that while short-term use may relieve anxious distress, longer exposure carries real risks for mood deterioration and suicidality in susceptible individuals.
This article explains how Klonopin affects mood, what the research shows, and how to use it safely if prescribed for depression-related symptoms.
What is Klonopin and How Does it Work?
Clonazepam belongs to the benzodiazepine class of medications. It enhances activity at GABA-A receptors in the brain, producing calming, anticonvulsant, and sedative effects. The FDA approved Klonopin primarily for seizure disorders and panic disorder, though doctors sometimes prescribe it off-label to manage anxiety and insomnia during the first weeks of antidepressant treatment.
As a long-acting benzodiazepine, clonazepam stays in the body for 20 to 50 hours. This extended half-life smooths out fluctuations between doses but can also lead to daytime sedation and cognitive slowing, particularly in older adults or at higher doses. The drug’s effects on inhibitory brain circuits can temporarily reduce hyperarousal and panic, yet these same mechanisms may dampen motivation and emotional responsiveness over time.
Can Klonopin Cause Depression?
Klonopin does not uniformly cause major depressive disorder in everyone who takes it. However, converging evidence indicates that clonazepam can precipitate or worsen depressive symptoms and increase suicidality risk in a meaningful subset of patients.
Direct Effects on Mood
The medication’s sedative properties can produce fatigue, reduced energy, slowed thinking, and emotional blunting. These effects often overlap with depressive symptoms, making it difficult to distinguish whether someone is experiencing medication side effects or an underlying mood disorder. Some patients also experience paradoxical reactions such as agitation, irritability, or disinhibition, which can increase distress and self-harm risk.
Pharmacovigilance Signals
Japan’s adverse drug event reporting system detected a strong clonazepam signal for suicide-related events, with a reporting odds ratio of 8.73. The signal was particularly elevated among females and adults in their 20s and 30s. A separate analysis of the FDA’s database found elevated suicidality reporting for several benzodiazepines compared with the sleep medication zolpidem, with higher rates in women and adults under 65 for specific agents.
Regulatory Warnings
The FDA requires clonazepam labels to include warnings about suicidal thoughts and behavior, consistent with the antiepileptic drug class. The prescribing information directs clinicians to monitor for emergence or worsening of depression, suicidality, or unusual mood changes, especially during the first few months of treatment.
Does Klonopin Help With Depression?
Short-term clonazepam use can improve certain depression-related symptoms, particularly anxiety and insomnia, during the first weeks of antidepressant treatment. A Cochrane review of 10 randomized trials found that adding a benzodiazepine to an antidepressant improved depressive severity, response, and remission rates during the early phase of treatment, defined as the first four weeks. However, these benefits disappeared in the acute phase of five to 12 weeks and beyond.
One double-blind trial tested low-dose clonazepam added to fluoxetine in 80 adults with major depression. The combination group showed faster improvement, achieving in four days what fluoxetine alone took 21 days to accomplish. Clonazepam particularly reduced early anxiety and sleep disturbance. Importantly, researchers tapered the clonazepam between days 21 and 33, avoiding prolonged exposure while preserving early gains.
These findings suggest a narrow therapeutic window: clonazepam may accelerate relief of anxious distress and insomnia during antidepressant initiation, but continuing beyond four weeks offers no sustained mood benefit and increases risk.
Klonopin Depression Risk Factors
Several factors increase the likelihood that clonazepam will contribute to mood problems:
- Duration of use: Suicide odds increased with the number of benzodiazepine dispensings in a healthcare system study of over 12,000 patients with anxiety or sleep diagnoses. Odds ratios rose from 1.66 for one to two fills to 5.64 for 15 or more fills.
- Sex and age: Pharmacovigilance data show higher suicidality reporting among women and younger adults taking certain benzodiazepines, including clonazepam.
- Polypharmacy: Taking multiple antiepileptic drugs or combining benzodiazepines with opioids substantially increases adverse neuropsychiatric outcomes and respiratory depression risk.
- Withdrawal and tapering: Abrupt discontinuation or rapid dose reduction can trigger severe withdrawal symptoms including anxiety, dysphoria, insomnia, and suicidality. The FDA label warns that withdrawal reactions can be life-threatening.

How Klonopin Affects Brain Chemistry and Stress?
Clonazepam’s effects on mood stem partly from its influence on stress-regulating brain circuits. GABAergic interneurons normally act as an inhibitory brake on the hypothalamic-pituitary-adrenal axis, which controls stress hormone release. When GABA-A signaling is disrupted, the HPA axis becomes overactive, elevating stress reactivity and contributing to depressive symptoms characterized by hyperarousal.
Research shows that GABAergic deficits drive HPA hyperactivity and produce behaviors resembling melancholic depression in animal models. PET imaging studies in PTSD patients document reduced benzodiazepine receptor binding, suggesting diminished GABA-A receptor availability in stress-related disorders.
Short-term GABA-A enhancement through clonazepam may temporarily restore inhibitory control over dysregulated stress circuits, theoretically improving anxiety and sleep while antidepressants take effect. However, long-term GABA-A potentiation risks tolerance, dependence, and cognitive impairment, potentially worsening mood through motivational blunting and reduced neuroplasticity.
Klonopin Safety Warnings and Risks
The FDA mandates a boxed warning for clonazepam highlighting three critical risk domains:
- Respiratory depression with opioids: Combining clonazepam with opioid medications can cause profound sedation, respiratory depression, coma, and death. The FDA label reserves such combinations only for cases where alternatives are inadequate and requires close monitoring.
- Abuse, misuse, and addiction: Clonazepam carries elevated overdose risk, often involving concomitant medications, alcohol, or illicit substances. Prescribers should assess risk before and during treatment.
- Dependence and withdrawal: Physical dependence can develop after weeks of consistent use. Abrupt discontinuation can trigger life-threatening withdrawal, including seizures in susceptible patients.
Additional safety considerations include:
- Avoiding alcohol and other central nervous system depressants
- Monitoring infants for sedation, poor feeding, and inadequate weight gain if breastfeeding
- Increased fall and cognitive impairment risk in older adults
- Memory effects that may interfere with learning and daily functioning
When Klonopin May Be Appropriate for Depression?
Clonazepam has a limited role in depression management, restricted to short-term adjunctive use in carefully selected cases. Appropriate scenarios include:
- Moderate to severe depression with prominent anxious distress or marked insomnia
- Starting an SSRI or SNRI with high risk of early activation or prior discontinuation due to anxiety
- Goal of accelerating early symptomatic relief during the two to four week window while the antidepressant establishes efficacy
Recommended approach:
- Use the lowest effective dose, typically 0.25 to 0.5 mg at bedtime or divided
- Plan tapering from the outset, beginning by week two to three
- Aim to discontinue by week four to six
- Reassess at weeks two and four using standardized measures
- If early improvement occurs, proceed with taper; if not, optimize the antidepressant strategy rather than extending benzodiazepine use
When to Avoid Klonopin?
Several situations warrant avoiding clonazepam or choosing alternatives:
- Active opioid use or prescription
- History of substance use disorder or benzodiazepine misuse
- During exposure-based trauma therapy, where benzodiazepines may impair fear extinction learning
- Roles requiring unimpaired memory and psychomotor performance
- Pregnancy or breastfeeding, where non-medication approaches should be prioritized
- Long-term mood management, given lack of sustained benefit beyond four weeks
A Delphi consensus of experts treating acute stress disorder in pilots specifically excluded clonazepam due to memory impairment and depression risk, preferring short-acting alternatives for brief use in operational settings.
Safe Discontinuation and Tapering
Gradual tapering is essential to minimize withdrawal and mood deterioration when stopping clonazepam. The 2025 Joint Clinical Practice Guideline on Benzodiazepine Tapering provides comprehensive recommendations for situations where benzodiazepine risks outweigh benefits.
Key tapering principles:
- Reduce dose by small increments every three to seven days, typically 10 to 25 percent of the daily dose
- Adjust the pace based on withdrawal symptoms
- If withdrawal emerges, pause the taper or return to the previous dose, then resume more slowly
- Coordinate with sleep hygiene and cognitive-behavioral strategies for insomnia and anxiety
- Consider non-benzodiazepine adjuncts if appropriate, though evidence for pharmacologic aids remains limited
Withdrawal symptoms can include rebound anxiety, insomnia, irritability, sensory hypersensitivity, and in severe cases, agitation and suicidality. These effects create a pathway by which clonazepam, through poorly managed discontinuation, can worsen depressive symptoms or trigger a depressive episode.
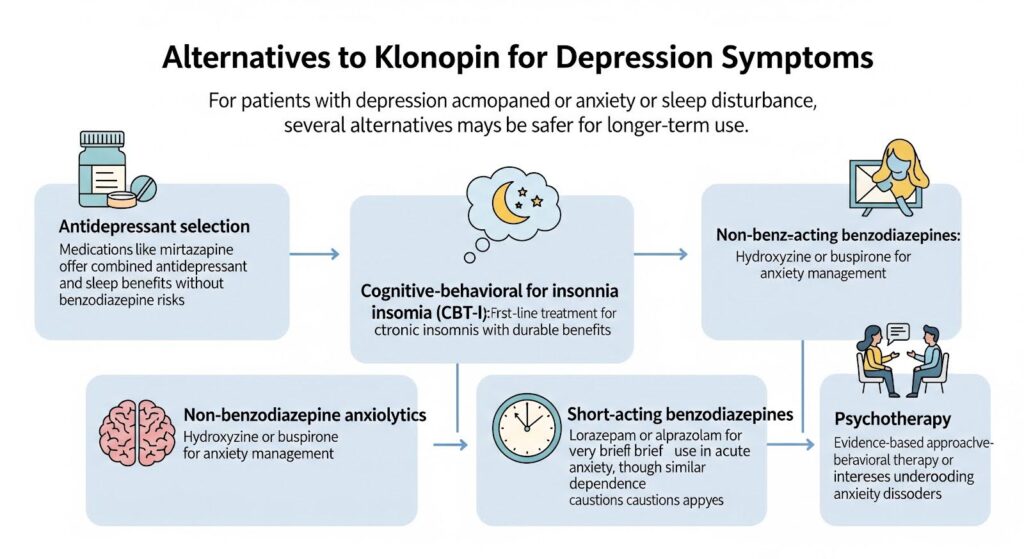
Alternatives to Klonopin for Depression Symptoms
For patients with depression accompanied by anxiety or sleep disturbance, several alternatives may be safer for longer-term use:
- Antidepressant selection: Medications like mirtazapine offer combined antidepressant and sleep benefits without benzodiazepine risks
- Cognitive-behavioral therapy for insomnia (CBT-I): First-line treatment for chronic insomnia with durable benefits
- Non-benzodiazepine anxiolytics: Hydroxyzine or buspirone for anxiety management
- Short-acting benzodiazepines: Lorazepam or alprazolam for very brief use in acute anxiety, though similar dependence cautions apply
- Psychotherapy: Evidence-based approaches like cognitive-behavioral therapy or interpersonal therapy address underlying mood and anxiety disorders
What the Research Shows?
The evidence base for clonazepam in depression comes primarily from older trials conducted before widespread SSRI use. Only two of the 10 trials in the Cochrane review used SSRIs, with the remainder testing tricyclic antidepressants. This limits direct applicability to modern practice, though the logic of bridging early SSRI activation remains clinically relevant.
A systematic review of neurosteroid GABA-A modulators in postpartum depression found low-certainty evidence for benefit, illustrating that targeting GABAergic tone can influence mood circuits but requires rigorous evaluation for safety and durability. These newer agents do not justify long-term benzodiazepine use in depression and highlight the need for safer, targeted GABAergic approaches.
Research gaps include:
- Modern pragmatic trials testing clonazepam augmentation with SSRIs and SNRIs
- Biomarker-guided selection to identify patients most likely to benefit
- Head-to-head comparisons of clonazepam versus short-acting benzodiazepines
- Optimized deprescribing protocols with behavioral supports
Clinical Bottom Line
Clonazepam occupies a narrow, time-limited role in depression management. It can accelerate early relief of anxiety and insomnia during the first weeks of antidepressant treatment, but benefits do not extend beyond four weeks. Prolonged use introduces substantial risks including dependence, cognitive impairment, and mood deterioration without durable antidepressant benefit.
The weight of evidence supports this approach:
- Use clonazepam selectively in low doses for two to four weeks maximum
- Target prominent anxious distress and insomnia during antidepressant initiation
- Plan and execute gradual tapering as soon as early stabilization occurs
- Avoid in high-risk situations including opioid co-prescribing, trauma therapy, and safety-sensitive roles
- Monitor closely for mood changes and suicidality, especially in women and younger adults
For patients struggling with depression and anxiety, comprehensive treatment combining evidence-based antidepressants, psychotherapy, and behavioral strategies offers the best path to sustained recovery without the risks of long-term benzodiazepine exposure.
If you or someone you care about is navigating depression with co-occurring anxiety or substance use concerns, professional support can make all the difference. Reach out to explore Summit’s dual diagnosis treatment options personalized to your needs.
