Overdose deaths in suburban Atlanta counties shifted dramatically when fentanyl infiltrated cocaine and methamphetamine supplies. Between 2022 and 2025, roughly two-thirds of fatal overdoses in counties like DeKalb involved fentanyl, often combined with stimulants.
This report synthesizes surveillance data from Georgia’s public health systems, CDC analyses, and regional intelligence to show how polysubstance risk evolved in Cobb, Gwinnett, Cherokee, Henry, and Clayton Counties, and what evidence-based strategies can reduce deaths in 2026.
The fentanyl–stimulant era has fundamentally altered overdose risk outside Atlanta’s urban core. After 2022 peaks, suburban counties likely saw stabilization in 2023–2024 due to intensified interventions, but the risk floor remains high. This article explains the data systems that track these trends, the mechanisms driving polysubstance mortality, and the county-specific actions needed to sustain progress.
Fentanyl Became the Dominant Driver in Suburban Overdose Deaths
Georgia’s Department of Public Health explicitly attributes the sharp increases in overdose deaths beginning in 2020 to fentanyl’s presence in stimulants like cocaine and methamphetamine. This mechanistic shift underpins the risk environment across suburban Atlanta counties from 2022 through 2025.
National mortality data confirm the pattern. The age-adjusted rate of deaths involving cocaine increased to 8.6 per 100,000 in 2023, while deaths involving psychostimulants with abuse potential rose to 10.6 in 2023. Critically, these increases have been primarily attributed to deaths co-involving opioids, with co-involvement dominating the stimulant-related mortality landscape.
In suburban counties such as Cobb, Gwinnett, Cherokee, Henry, and Clayton, three phenomena defined risk from 2022 to 2025: peak or near-peak mortality levels around 2022 shaped by fentanyl-stimulant co-involvement; general stabilization or modest declines in 2023–2024 associated with increased naloxone availability and early fentanyl test strip integration; and a persistent, structurally entrenched polysubstance environment complicated by the emergence of xylazine and nitazenes.
How Surveillance Systems Track Polysubstance Risk?
Understanding suburban overdose trends requires integrating multiple data streams that differ in scope, timeliness, and specificity. Georgia’s OASIS mortality system provides final, residence-based county counts and rates for drug overdoses through the most recent completed year. Definitions follow NCHS ICD-10 standards, with small-number suppression to protect privacy.
CDC’s State Unintentional Drug Overdose Reporting System captures detailed toxicology and circumstances for unintentional and undetermined overdose deaths. Public dashboards emphasize state-level trends, but county-specific interpretation can be triangulated through OASIS and local reporting.
Emergency department surveillance operates through two complementary systems. DOSE-SYS provides near-real-time suspected overdose signals from chief complaint and triage text, enabling rapid cluster detection. DOSE-DIS offers lagged but validated ED and inpatient discharge data with drug categories including opioids, fentanyl, methamphetamine, and cocaine, updated annually with roughly eight-month lag.
These systems are essential because nonfatal overdose trends can diverge from mortality due to naloxone saturation and improved clinical response. ED visits may rise even as deaths stabilize, reflecting successful life-saving interventions rather than worsening risk.
Suburban County Patterns Showed Stabilization After 2022 Peaks
DeKalb County provides the clearest window into suburban trends. Publicly reported county figures indicate total overdose deaths increased from 142 in 2020 to 217 in 2023, then declined to 203 in 2024, a 6.5% decrease. Importantly, roughly 65 to 70% of deaths involved fentanyl across recent years, essentially two-thirds of all fatalities.
This level of fentanyl penetration matches or exceeds Georgia’s statewide synthetic opioid share, which stood at approximately 63% in 2024. The pattern underscores fentanyl’s dominance in DeKalb’s overdose landscape and suggests similar dynamics in neighboring suburban counties.
Gwinnett County’s 2024 age-adjusted death rate due to all drug overdose stood at 12.4 per 100,000, below the Georgia state value. Historical news coverage showed fentanyl-related deaths nearly tripled from 2019 to 2020, indicating early and significant impact in suburban settings as counterfeit pills proliferated.
Cobb County experienced steep increases through 2022, followed by the first stabilization and decline in 2023 across several age groups, with provisional signs continuing into 2024. Fentanyl involvement remained substantial, and demographic shifts included rising burden among Hispanic residents, indicating the need for multilingual outreach and culturally tailored interventions.
Why Stimulant Users Face Unexpected Opioid Toxicity?
Georgia’s Department of Public Health issued a March 31, 2022 alert after increased overdoses from drugs mixed with fentanyl, particularly cocaine, methamphetamine, and counterfeit pills. At least 66 ED visits were reported from early February to mid-March; some stimulant overdoses responded to naloxone, indicating hidden fentanyl exposure.
These clinical anecdotes translate to a durable surveillance concern. Non-opioid-identifying populations, such as stimulant users, face unexpected opioid toxicity, shifting outreach needs and naloxone placement strategies. Whether via counterfeit pills sold as oxycodone or alprazolam consumed by stimulant-preferred users, or via direct contamination of cocaine and methamphetamine, the pharmacologic mismatch increases respiratory depression risk and complicates recognition and response, especially among persons with low opioid tolerance.
DEA’s Atlanta Division reported seizing about 40,000 fentanyl-containing pills in 2024, more than double 2023, and roughly 600 pounds of fentanyl powder. Nationally, about half of pills tested by DEA in 2024 contained a potentially lethal dose. These seizures imply a rich local market for illicitly manufactured fentanyl and counterfeit pills, increasing the probability that non-opioid users encounter fentanyl inadvertently.
Racial Disparities Require Targeted Suburban Strategies
From 2018 to 2023, psychostimulant-involved deaths rose most among non-Hispanic American Indian and Alaska Native persons, and cocaine-involved deaths rose most among non-Hispanic Black persons, while both groups experienced increasing stimulant–opioid co-involvement. In southern and western markets where fentanyl proliferated later, these increases accelerated more recently.
For metro Atlanta, this implies sustained focus on Black communities for cocaine–fentanyl risk and targeted prevention messaging responsive to cultural and occupational contexts. Suburban counties with substantial Black communities, such as southern and eastern Gwinnett, south Cobb, and Clayton, should prioritize culturally tailored engagement, targeted naloxone and fentanyl test strip distribution, and gateway service points trusted by Black communities.
Detailed toxicology analyses reveal meaningful differences between stimulant-only deaths and stimulant–opioid co-involved deaths. Decedents in stimulant-only cases had higher prevalence of cardiovascular disease (38.7% vs. 21.2%) and were more often seen in the ED for the fatal event (33.1% vs. 18.4%), while stimulant–opioid co-involved decedents had more evidence of opioid use history and prior treatment exposure.
These distinctions matter in Atlanta, where cocaine markets intersect with Black communities and methamphetamine use has spread more broadly. Clinical teams should anticipate different comorbidity profiles and engagement histories by co-involvement status.

Emerging Adulterants Complicate Overdose Response
National forensic laboratory data confirm that methamphetamine and fentanyl dominate drug evidence. In 2022, methamphetamine accounted for 341,049 reports and fentanyl 163,201, with significant counts of fluorofentanyl (22,242), xylazine (9,125), and cocaine (169,972). The breadth of lab participation supports representativeness across the national drug caseload.
Quarterly snapshots document the arrival of novel nitazenes in 2024 and 2025 and ongoing fentanyl analog variability, providing reason to anticipate a persistent, evolving fentanyl-stimulant risk environment across Georgia’s metro and suburban corridors.
Xylazine, a veterinary sedative, has spread within illicitly manufactured fentanyl supplies nationwide, complicating overdose presentations with prolonged sedation and necrotic skin wounds and weakening response to naloxone for the non-opioid component. A 2024 analysis demonstrated that xylazine-involved death rates doubled between 2021 and the first quarter of 2024, and that racial inequalities widened, with Black populations experiencing elevated rates.
While fentanyl remains the primary risk, metro Atlanta surveillance should incorporate xylazine monitoring and consider wound care and sedation management protocols within ED and harm reduction settings.
Evidence-Based Interventions Can Sustain Mortality Reductions
The 2024 mortality declines in parts of the metro are real but modest, and they coexist with ongoing nonfatal ED burden. Without continued investment in naloxone, fentanyl test strips, medications for opioid use disorder, and stimulant-specific care, aligned with granular, integrated surveillance, mortality could plateau at an unacceptably high level or rebound with the next supply shock.
Naloxone Saturation and Leave-Behind Protocols
Widespread naloxone distribution through EDs, EMS, community-based organizations, and pharmacies increases survival and likely contributes to divergence between ED and mortality trends. Leave-behind programs, where EMS and ED staff provide naloxone kits to overdose survivors and their networks, are essential features of suburban response systems.
Training non-traditional partners, including workplaces, transit systems, and hospitality venues, is crucial in metro settings. Georgia’s Department of Public Health emphasizes immediate naloxone use and calling 911 as core public messages, reflecting real-world necessity in an era of unpredictable potency and poly-adulteration.
Fentanyl Test Strips and Drug Checking
Scaling up fentanyl test strip distribution beyond opioid-user networks to stimulant-using communities is justified by risk profiles in urban and suburban corridors. Clear guidance on proper sampling, interpretation limits, and repeated testing across a batch is essential. Non-detection is not proof of absence, and xylazine and other non-opioids are not detected by fentanyl strips.
Georgia’s opioid settlement funds have supported FTS distribution by multiple organizations. Drug checking equipment can reduce overdose deaths when integrated with transparent education about limitations and paired with naloxone access.
Medications for Opioid Use Disorder and Contingency Management
Expanding low-barrier buprenorphine and methadone access, including same-day starts in EDs and withdrawal management in county jails with continuity to community care, directly addresses fentanyl-involved mortality. For stimulant use disorder, contingency management is the most evidence-based behavioral intervention. Piloting and scaling contingency management in county programs can directly address stimulant co-involvement risk.
County-level declines, where present, correlate with targeted interventions: naloxone leave-behind programs, ED-based naloxone distribution, peer navigators, immediate MOUD initiation, and post-discharge follow-up. These interventions are more likely to be robust in core suburban counties with large hospital hubs.
Data Integration Enables Rapid Response to Emerging Threats
To track 2025 conditions locally, counties should use OASIS for final county deaths, triangulate with DOSE-SYS monthly trends and DOSE-DIS annual validation, and consult provisional state-level indicators to understand synthetic opioid shares. Georgia’s Drug Surveillance Unit provides monthly and quarterly reports across these streams and can coordinate local data-to-action cycles with district analysts.
A standard operating picture includes weekly DOSE-SYS suspected overdose trends, cross-checked with EMS runs including naloxone use to identify emerging hotspots at the neighborhood level. Monthly triangulation with provisional indicators and queries to state analysts for notable shifts in ED patterns by county supports rapid operational decisions.
Quarterly validation against DOSE-DIS updates where available and annual updates to county-level overdose mortality maps and rankings, with assessment of changes by age, race, ethnicity, and sex, inform settlement fund investments and community coalition priorities.
Public dashboards and regular briefings maintain community trust. Disaggregation by race, ethnicity, age, and geography should guide resource allocation to address disparities and evolving hotspots.
County-Specific Readiness and Risk Posture
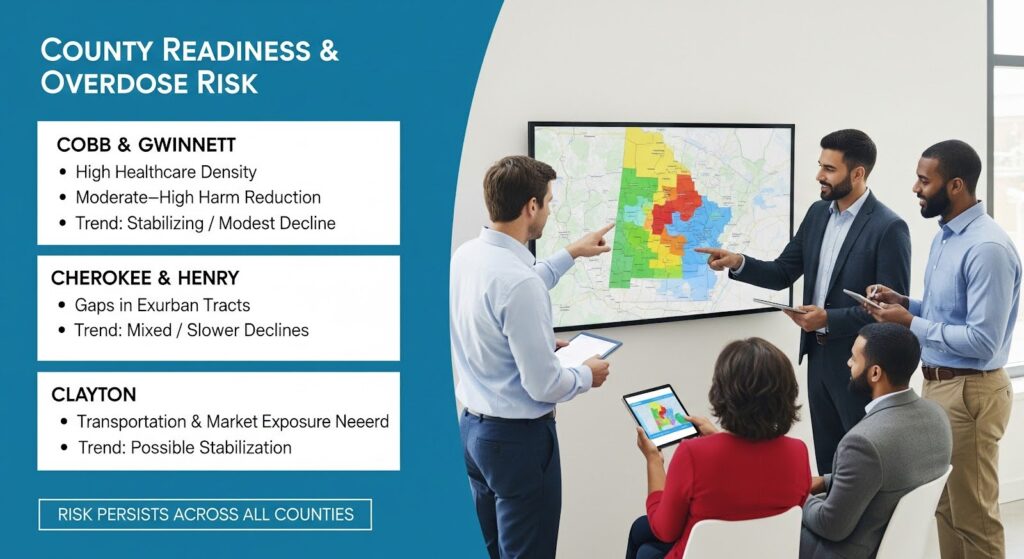
Cobb and Gwinnett are populous, diverse core suburban counties with extensive healthcare systems and public safety infrastructure. High healthcare hub density and moderate to high harm reduction and fentanyl test strip integration support stabilization or modest declines, but elevated risk persists and requires continued integration.
Cherokee and Henry represent fast-growing exurban corridors with substantial commuting populations and evolving service density. Moderate healthcare hub density and moderate harm reduction integration, with gaps in exurban tracts, suggest mixed trends with possible slower declines. Elevated steady state risk requires infrastructure growth, particularly for methamphetamine and fentanyl vigilance.
Clayton, adjacent to the urban core and the airport corridor, features mixed socioeconomic profiles and regional transportation dynamics that can accelerate market exposure. Moderate healthcare hub density and moderate harm reduction integration, with targeted outreach needed, support possible stabilization, but elevated risk requires sustained community engagement.
Why Suburban Strategies Must Address Polysubstance Complexity?
The central policy imperative is to institutionalize dual-track strategies: sustain life-saving nonfatal responses while removing barriers to durable, evidence-based treatment for both opioid and stimulant use disorders. The fentanyl–stimulant polysubstance era is the new normal in the Atlanta suburbs. Responses that match its complexity can drive durable reductions in overdose mortality.
Suburban counties should sustain naloxone saturation with stimulant-focused targeting, ensuring naloxone is universally accessible in stimulant networks and expanding leave-behind programs countywide. Normalizing fentanyl test strips in pharmacies and community channels, with formalized stocking agreements and multilingual instructions integrated with overdose education, scales risk mitigation.
Expanding MOUD access with low-barrier models, extending office-based buprenorphine in primary care networks and deploying mobile and telehealth options to exurban tracts, addresses the opioid component of polysubstance risk. Investing in contingency management for stimulant use disorder, building capacity across suburban behavioral health systems and pairing with case management, addresses the stimulant component.
Building integrated dashboards that combine OASIS, provisional indicators, SUDORS, EMS, and regional intelligence feeds, with monthly multi-agency coordination calls to respond to emergent analogs, enables counties to shift from retrospective reporting to forward-leaning prevention.
Equity-forward targeting directs resources to census tracts with higher socioeconomic vulnerability and lower educational attainment, tailoring outreach in areas with large Black populations at high risk for cocaine and fentanyl co-involvement. Strengthening operational ties between regional intelligence centers and state public health, with predefined triggers for rapid response, anticipates supply shocks.
If you or someone you know is navigating the challenges of polysubstance use in the Atlanta area, compassionate, evidence-based care is available. Reach out to explore Summit’s addiction counseling options that integrate medications for opioid use disorder, contingency management for stimulant use, and holistic support personalized to your needs.
