High-achieving professionals in Atlanta face a perfect storm of workplace stress, residential safety concerns, and access to controlled substances that can quietly fuel addiction while outward performance remains intact.
Recent data show that federal return-to-office mandates clash with worker preferences and physical space realities, eroding morale and autonomy precisely when Metro Atlanta’s opioid burden remains the highest in Georgia.
This article explains how workplace policies, urban stressors, and behavioral health system gaps converge to elevate risk for professionals who maintain careers while concealing substance misuse, and what Atlanta can do to detect and support these individuals earlier.
What Makes High-Functioning Addiction Hard to Spot in Professionals?
High-functioning addiction describes patterns of substance misuse that meet clinical criteria for a disorder yet coexist with preserved job performance, stable relationships, and absence of obvious red flags.
In safety-sensitive professions like healthcare, law, and aviation, task performance has narrow margins for error. The combination of role expectations and fear of licensing repercussions drives concealment, delayed disclosure, and minimization, elevating latent risk to public safety.
Evidence indicates that prevalence of substance use disorder among healthcare professionals is broadly similar to the general population at about 10 percent, although misuse more frequently involves alcohol and addictive medications such as sedatives and opioids, reflecting differential access and professional culture.
Within Metro Atlanta, this challenge is amplified by a metropolitan behavioral health profile that diverges significantly from state and national patterns across multiple measures, paired with a professional environment where help-seeking may be impeded by confidentiality concerns, program costs, and variable standards.
Atlanta’s Workplace Stress is Intensifying for Federal and Corporate Employees
Atlanta’s large federal workforce is navigating a renewed return-to-office mandate under conditions that increase practical stress and diminish perceived autonomy. Many agencies shed office space during the pandemic, and now piling back into the office just isn’t doable, at least if everyone wants a desk.
This creates logistics friction and daily uncertainty. Commercial real estate experts and federal worker unions note that uniform mandates may run afoul of negotiated telework terms, compounding employee frustration and legal tension.
Workers report fear of reduced effectiveness, morale killing, and the risk of talent loss if hybrid flexibility is curtailed. The American Federation of Government Employees emphasizes the importance of hybrid arrangements for attracting and retaining key talent.
Sudden reductions in control and predictability are classic stress amplifiers for professionals, heightening reliance on coping strategies that can evolve into misuse, particularly when performance expectations remain high while support and resources feel diminished.
Meanwhile, the metropolitan office sector shows high vacancies and distress, albeit with some 2024 leasing momentum. Emptier offices depress building values, affecting landlords, ground-floor retail, and potentially local tax collections.
Older, struggling buildings may face conversion to residential or demolition, and such transitions can prolong uncertainty for tenants and workers. Uncertain office footprints and shifting building uses affect commuting patterns, meeting cadence, and inter-team coordination, creating friction that can perpetuate stress even as organizations attempt to normalize operations.
Adding to the anxiety, Coca-Cola announced plans for corporate layoffs in Atlanta in January 2026, affecting about 2.5 percent of headquarters staff. High achievers do not interpret macro job gains uniformly; sector-specific restructuring influences perceived job insecurity.
In high-performance cultures, fear of being next can drive compulsive work patterns and reliance on performance-enhancing or anxiety-dampening substances, especially when organizational supports are tight and hybrid flexibility is under challenge.
Residential Safety and Nightlife Risks Add Environmental Stress
Even high-achieving professionals can be renters in areas affected by concentrated violent crime, especially those early in careers or preferring proximity to urban amenities. The Atlanta Journal-Constitution’s dangerous dwellings database documents persistent violent crime at specific multifamily addresses across 2017 to 2023, paired with housing code violations.
Examples include properties recording dozens of aggravated assaults and multiple homicides. One 240-unit complex logged 66 aggravated assaults from 2017 to 2019; others report 42, 37, 31, 25, and 11 aggravated assaults. Individual incidents highlight chronic exposure to violence, including shootings that injured teens, shots fired into apartments with children present, and homicides.
Code complaints include exposed wiring, structural damage, leaks, raw sewage, rats, lack of air conditioning, and safety hazards; some properties received failing or low HUD inspection scores.
Daily exposure to violent incidents, code deficiencies, or publicized threats significantly elevates baseline anxiety. Compounded with work stress, this creates a two-front strain that can make maladaptive coping, including substance use, more likely to persist unnoticed, particularly if daytime functioning remains intact.
Atlanta’s entertainment economy is robust, but several developments introduce acute safety concerns at nightlife venues. The city’s major music festival, Music Midtown, was canceled due to Georgia’s permitless concealed-carry law preventing organizers from banning firearms on public property, prompting safety concerns about mixing guns and alcohol and an estimated $50 million economic loss.
A mass shooting at The Masquerade saw two intoxicated individuals with handguns open fire, killing two and injuring two, illustrating consequences when intoxication and firearms intersect at venues frequented by young professionals.
Professionals often use nightlife as stress relief. Elevated risk environments where alcohol is prevalent and firearms may be present create both immediate safety risks and a culture of high-intensity substance use.
This is not to assert causality; rather, the environment normalizes heavier episodic consumption and increases trauma exposure risk. Over time, a subset of high performers may escalate use patterns while maintaining outward professional performance, fitting the high-functioning profile.
Metro Atlanta’s Behavioral Health Profile Differs from State and National Benchmarks
SAMHSA’s Metro Brief specific to Atlanta–Sandy Springs–Marietta uses annual averages over 2005 to 2010 and states that any higher or lower statements versus Georgia or U.S. estimates are statistically significant at 0.05.
Population denominators average 4.195 million aged 12 and older and 3.737 million aged 18 and older in the MSA, ensuring adequate base for interpreting estimates.
A companion tables file provides exact rates, 95 percent confidence intervals, p-values, and estimated numbers, enabling precise extraction for measures such as binge alcohol use, marijuana use, and nonmedical pain reliever use.
While dated, these MSA-specific estimates remain the most recent publicly available MSA-level snapshot of Atlanta’s behavioral health profile and establish that the Atlanta MSA’s differences in multiple measures were not due to chance alone.
The presence of multiple statistically significant differences means stakeholders cannot assume the MSA mirrors state or national averages.
Georgia’s recent model-based estimates provide updated, albeit statewide, quantitative context for Atlanta. For 2022 to 2023, Georgia reported among people aged 12 and older marijuana use in the past year at 1,815 thousand, marijuana use in the past month at 1,209 thousand, illicit drug use in the past month including marijuana at 1,374 thousand, illicit drug use other than marijuana in the past month at 320 thousand, and cocaine use in the past year at 146 thousand.
These totals, particularly for marijuana and illicit drug use, indicate substantial statewide exposure. Although these are not MSA-specific, Atlanta’s population share and historic metro divergences suggest these statewide figures likely understate true Atlanta MSA prevalence.
Opioid Burden Remains Concentrated in Metro Atlanta
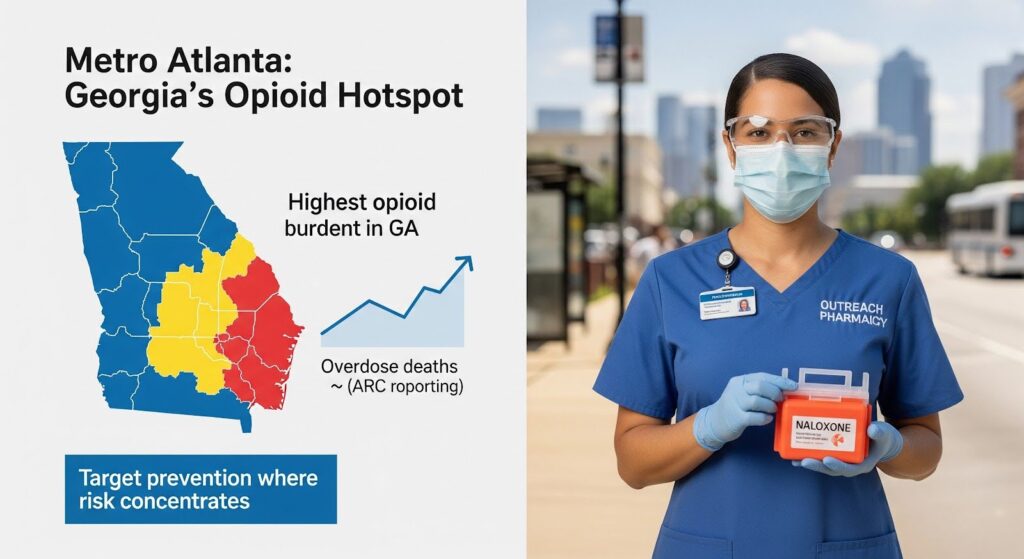
Two complementary data streams underscore a long-standing and evolving opioid burden in Metro Atlanta. Prior to the COVID-19 pandemic, Metro Atlanta was reported to have the highest opioid use in Georgia, suggesting a persistent regional burden relative to the rest of the state.
The Atlanta Regional Commission further documented rising opioid overdose deaths in the Metro region, reinforcing the salience of opioids as a strategic area for prevention and rapid response.
Peer-reviewed work focusing on Metro Atlanta demonstrates that wastewater-based epidemiology can provide near real-time, community-level measures of opioid exposure, functioning as an early-warning or situational awareness system to complement overdose surveillance and guide harm reduction resource allocation.
The public health utility is twofold: detect shifts in community-level exposure such as fentanyl surges or geographic hotspots, and inform targeted, time-sensitive deployment of naloxone, outreach, and pharmacy engagement for harm reduction. For an MSA like Atlanta, wastewater-based epidemiology’s temporal resolution and community specificity offer tangible operational advantages over annual survey cycles.
Why Professionals Delay Seeking Help Despite Available Programs?
Fear of disclosure to licensing boards is a major deterrent to help-seeking; more than 40 percent of physicians report not seeking help for burnout or depression due to this concern. The American Medical Association and allied organizations have advocated for narrowing or eliminating problematic licensing questions that inquire broadly about past diagnosis or treatment rather than current impairment.
In Georgia, evolving communication about Professional Health Program confidentiality indicates national momentum to clarify what information is shared, when, and under what conditions. Increased clarity and fidelity to impairment-focused inquiries are essential to reduce stigma and encourage early engagement.
Georgia’s Professional Health Program is funded by participant fees mandated by law and accepts donations; participants bear all costs associated with participation. For high-functioning professionals, the prospect of significant out-of-pocket costs, extended monitoring, and obligations can discourage early voluntary entry.
Parity legislation seeks to enforce equitable coverage for mental health and substance use disorder, but operationalizing parity for program-adjacent services such as evaluations and monitoring can be complex. Nonetheless, parity enforcement and complaint repositories now exist to identify and address insurer barriers.
Program variability across states and across professions complicates expectations around duration, monitoring intensity, and return-to-work, creating uncertainty that can also dissuade engagement. Georgia Professional Health Program rules provide that all records are confidential, not subject to court subpoena or discovery, and used only in exercise of program functions.
However, noncompliance with program recommendations results in forwarding information to the Board. The Board retains authority to use program information in proceedings consistent with Georgia law. This dual structure, strong confidentiality protections with explicit noncompliance reporting, represents both a protection and deterrent.
For high-functioning professionals, the perceived risk of being locked into a structured, reportable process if any deviation occurs may impede seeking help until crises arise.
Encouragingly, the program aims to restore safe practice, not punish, and national program outcome data indicate high abstinence and work retention, messages that should be proactively communicated to reframe participation as a path to long-term safety and career preservation.
Georgia’s Mental Health Parity Act Can Reduce Financial Barriers
Georgia’s Mental Health Parity Act, signed April 4, 2022, implements recommendations of the Georgia Behavioral Health Reform and Innovation Commission and enforces compliance with federal parity for mental health and substance use disorder.
It requires insurers to provide equitable coverage, defines medical necessity, mandates annual parity compliance reviews and data calls, establishes complaint repositories, and prohibits same-day reimbursement bans for mental health and primary care visits. It also supports workforce initiatives and accountability courts.
For high-functioning professionals, the law strengthens pathways to covered care and provides recourse when nonquantitative treatment limitations inappropriately block access, an important shift for financially deterring barriers.
Annual unified reports via the Georgia Data Analytics Center and Department of Behavioral Health and Developmental Disabilities compliance reports create transparency and enforcement opportunities.
Warning Signs That Colleagues and Employers Should Watch For
Because high-functioning individuals maintain outward productivity and interpersonal stability, detection relies on subtle, patterned deviations rather than dramatic impairment. Individual performance indicators include slight increases in charting errors, lapses in attention, or pattern inconsistency in clinical or analytical tasks that previously were executed flawlessly.
Variability in work output and affect, alternating periods of unusually high productivity with unexplained fatigue, irritability, or presenteeism, can signal trouble. Discreet risk management behaviors such as overreliance on colleagues to double-check work without transparent rationale or avoidance of high-stakes tasks at certain times of day are also red flags.
Changes in self-care, shifts in sleep, appetite, or physical appearance masked by schedule intensity, and increased use of functional substances to modulate performance and recovery between shifts warrant attention.
Workplace and systems-level red flags include controlled substance access irregularities, anomalies in medication handling logs, pharmacy discrepancies, or repeated just-in-time refills without clinical justification in safety-sensitive settings.
Chronic overtime or self-assignment to isolated tasks where supervision is minimal, framed as commitment but functioning as concealment, is another pattern. Departures from usual collegiality, subtle defensiveness about schedule or whereabouts, and increased privacy about breaks or post-shift activities should prompt concern.
Explicit reluctance to use employee assistance programs or mental health benefits due to fear of disclosure is validated by national data.
What Atlanta Employers and Agencies Can Do Now?
Make confidentiality explicit and credible by publishing a Georgia Professional Health Program transparency suite that covers confidentiality boundaries, monitoring steps, noncompliance consequences, costs, and typical durations, mapped to national standards.
Emphasize the program’s goal of safe return to practice and high abstinence and work-retention outcomes. Align licensing and credentialing questions to current impairment only; audit hospital privileging forms and malpractice applications to harmonize language.
Reduce financial friction by leveraging parity enforcement for mental health and substance use disorder coverage. Establish a dedicated hardship fund, donation-supported, for program monitoring costs to encourage voluntary early entry. Consider employer co-funding pilots in safety-sensitive sectors to reduce individual financial burden.
Integrate surveillance with engagement by creating an Atlanta Professional Behavioral Health Dashboard that overlays wastewater-based epidemiology signals, overdose trends, and de-identified program intake timing to drive targeted, stigma-free outreach. Partner with pharmacies for community-level harm reduction aligned with wastewater-based epidemiology spikes.
Standardize and evaluate aftercare and return-to-work by adopting national best practice guidelines statewide. Publish standardized return-to-work criteria and monitoring tiers with explicit rationale, borrowing aviation’s phased logic adapted for healthcare and legal professions. Launch a statewide outcomes registry, de-identified, to measure abstinence, relapse, and work retention over five years.
Expand low-friction entry points by offering confidential, anonymous screenings via QR codes in professional spaces such as hospitals, courthouses, and conference centers, with direct linkage to program navigation. Ensure 24/7 live support with discreet appointment scheduling compatible with professionals’ schedules.
Build capacity for subacute stabilization by aligning adult residential mental health program capacity with professional needs, such as privacy-preserving environments, flexible visitation for legal counsel, and embedded occupational therapy, and create smooth handoffs to program monitoring.

Why This Matters for Atlanta’s Future?
Atlanta’s high-achieving professionals operate within a behavioral health environment characterized by demonstrable MSA-level divergences from state and national benchmarks historically, significant and persistent statewide substance use magnitudes, a documented regional opioid burden, and access to innovative surveillance like wastewater-based epidemiology.
Among safety-sensitive professions, help-seeking is suppressed by confidentiality concerns, financial burdens, and program variability, even though structured monitoring programs demonstrably support abstinence and safe return-to-work.
In this context, the most impactful near-term actions are those that increase the credibility and clarity of confidentiality promises and impairment-focused licensing practices, reduce out-of-pocket burdens by enforcing parity and creating co-funding options, operationalize wastewater-based epidemiology to guide targeted outreach and harm reduction, and standardize aftercare and return-to-work expectations aligned with national guidance, evaluated via outcomes registries.
Updating the MSA evidence base for Atlanta is equally important, yet not a prerequisite for action, given the convergence of signals.
The integration of these measures is likely to surface hidden cases earlier, reduce crisis-driven detection, protect patient and client safety, and sustain professional careers, outcomes that benefit individuals, employers, and the broader Metro Atlanta community.
If you or a colleague is navigating the pressures of high performance alongside substance use concerns, confidential support is available. Reach out to explore Summit Wellness Group’s addiction treatment options designed for professionals who need flexible, evidence-based care without compromising career goals.
