Middle-aged professionals in Atlanta face mounting pressures, demanding careers, caregiving responsibilities, and the lingering stress of pandemic disruptions.
These forces can quietly reshape drinking habits, turning occasional happy hours into patterns that threaten health and performance. Between 2016 and 2021, deaths from excessive alcohol use in the United States surged 29.3%, climbing from roughly 138,000 to 178,000 annually, with chronic conditions like liver disease driving two-thirds of fatalities.
For Atlanta’s professional workforce, this national crisis likely mirrors local realities: alcohol misuse among middle-aged adults appears to have increased during the pandemic and remains a pressing occupational health issue.
This article examines the evidence, explores the causes, and outlines practical steps for employers and individuals to address the problem.
What the National Data Reveals About Alcohol Misuse Trends?
The Centers for Disease Control and Prevention (CDC) documented a sharp escalation in alcohol-attributable deaths during the pandemic. Age-standardized death rates rose from 38.1 per 100,000 in 2016–2017 to 47.6 per 100,000 in 2020–2021.
The increase was modest before COVID-19 hit, just 5.3% between 2016–2017 and 2018–2019, but then jumped 22.8% as the pandemic took hold. Women experienced a proportionally larger increase, with deaths rising 34.7% compared to 26.8% among men.
Chronic causes dominated the toll. Rates of chronic alcohol-related deaths climbed from 23.2 to 29.4 per 100,000 across the study periods, reflecting conditions like alcoholic liver disease, pancreatitis, and certain cancers that develop over years of sustained heavy drinking. For professionals in their 40s, 50s, and early 60s, these figures signal a long-term health threat that extends far beyond the immediate risks of a single binge episode.
Emergency department visits involving acute alcohol consumption also increased during 2018–2020, according to the National Institute on Alcohol Abuse and Alcoholism. By 2020, alcohol was implicated in at least 7.1% of all ED visits. Earlier national data showed a 47% rise in alcohol-related ED visit rates between 2006 and 2014, with particularly notable increases among adults aged 45 and above.
Binge Drinking Patterns in Midlife Adults
Behavioral surveys reveal troubling patterns among older adults. Research on adults aged 40–64 found strong associations between high-intensity binge drinking and concurrent cigarette smoking or e-cigarette use.
High-intensity binge drinking, consuming far more than the standard binge threshold, clusters with nicotine use, amplifying cardiovascular and respiratory risks.
The National Institute on Alcohol Abuse and Alcoholism defines binge drinking as consuming five or more drinks for men, or four or more for women, in roughly two hours, levels that typically raise blood alcohol concentration to 0.08%. Among binge drinkers nationally in 2018, the median frequency was 1.7 occasions per month, and the median intensity was 5.5 drinks per occasion.
However, a small subset drank far more heavily, with 90th percentile values reaching 9.5 occasions per month and 11.5 drinks per occasion.
Studies tracking older adult drinking trends from 2015 to 2019 documented persistent binge drinking prevalence in this age group, with some analyses suggesting larger increases among adults 45 and older compared to younger cohorts.
These patterns predate the pandemic, indicating that midlife professionals entered 2020 with an already elevated baseline of risky drinking.
Atlanta’s Local Context and Surveillance Capacity
Georgia’s OASIS emergency department data system provides a powerful tool to track alcohol-related harms at the county level.
The system captures ER visits by Georgia residents treated at in-state, non-federal hospitals, with stratification by age, sex, and principal diagnosis. For middle-aged adults, those aged 45–64, OASIS can monitor trends in conditions like alcoholic liver disease and mental and behavioral disorders due to alcohol.
The system relies on billing data and principal diagnosis coding, which may undercount alcohol involvement in some injury visits.
Additionally, it excludes Georgia residents treated out of state. Despite these limitations, OASIS offers age-adjusted and deduplicated visit measures that support robust trend analysis when methodological caveats are applied.
Local behavioral surveillance comes from the Behavioral Risk Factor Surveillance System’s SMART (Selected Metropolitan/Micropolitan Area Risk Trends) reports.
These provide metropolitan statistical area-level estimates of binge drinking by age group for the Atlanta–Sandy Springs–Roswell MSA through 2015. However, BRFSS underwent a major redesign in 2011, adding cell phone sampling and new weighting methods, so pre-2011 estimates are not directly comparable to later years.
Together, OASIS and SMART BRFSS enable triangulation: behavioral baselines through 2015, followed by ER harm proxies during the critical 2019–2021 pandemic period.
Why Alcohol Misuse Likely Rose During the Pandemic?
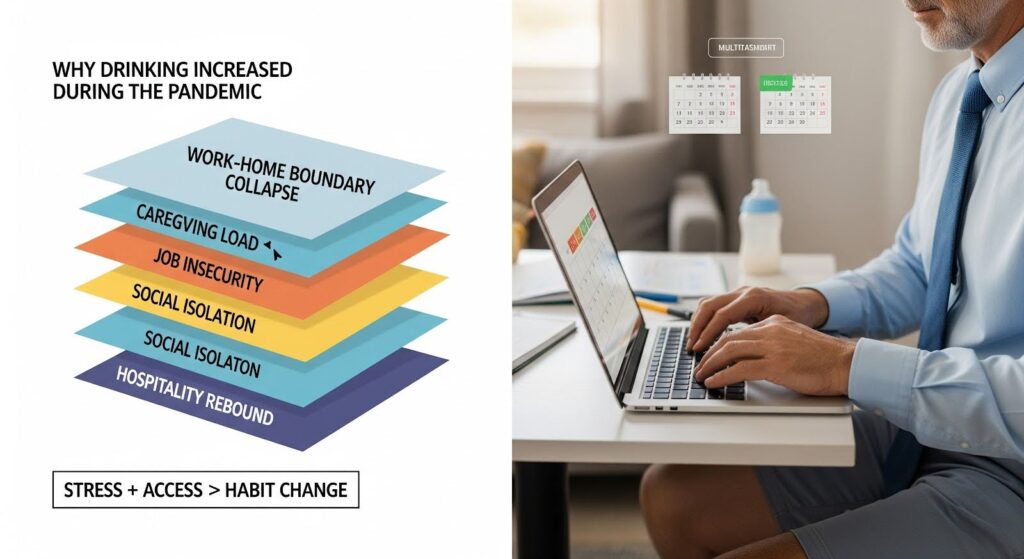
Multiple forces converged to elevate drinking risks among middle-aged professionals during the pandemic.
Physician commentary summarizing consumer surveys found that 31% of respondents increased their drinking frequency, 16% raised their typical quantity by about two drinks, and 27% consumed more than four additional drinks on heavier days. While not population-representative, these patterns align with national mortality and ED trends.
Work-related stressors intensified. Remote work blurred boundaries between professional and personal time, while caregiving demands surged for those managing children’s virtual schooling or aging parents’ health needs.
Social isolation and anxiety about job security compounded the pressure. For some professionals, alcohol became a coping mechanism, a way to unwind after Zoom-heavy days or to manage uncertainty.
Atlanta’s hospitality sector rebounded sharply after initial pandemic closures. Employment in food services and drinking places in the Atlanta MSA climbed from 196,000 in 2020 to 243,100 by 2024. This expansion signals increased availability of social drinking venues and a return to alcohol-centered networking events, contexts that can normalize and sustain regular consumption among professionals.
The clustering of high-intensity binge drinking with nicotine use among adults aged 40–64 suggests that some professionals may engage in multiple risk behaviors simultaneously, particularly when under stress.
This co-use pattern raises the stakes for cardiovascular events, respiratory complications, and accelerated progression of chronic conditions.
Health Impacts for Middle-Aged Professionals
The predominance of chronic causes in alcohol-attributable deaths carries profound implications for midlife adults. Sustained heavy drinking increases the risk of alcoholic liver disease, which can progress to cirrhosis.
It also elevates the risk of alcohol-attributable cancers, including breast cancer in women and cancers of the oral cavity, pharynx, esophagus, liver, and colon.
Women face disproportionate harm. The 34.7% increase in female alcohol-attributable deaths between 2016–2017 and 2020–2021 reflects both rising consumption and sex-specific vulnerabilities.
Women metabolize alcohol differently than men, and they are more susceptible to liver damage at lower levels of consumption. For female professionals in midlife, even moderate sustained increases in drinking can translate into substantial long-term risk.
Acute harms also matter. Emergency department visits involving alcohol often stem from injuries, poisonings, or mental health crises. For professionals, these events can disrupt work continuity, damage reputations, and trigger downstream consequences like impaired driving arrests or falls.
The 7.1% of ED visits involving alcohol in 2020 underscores the healthcare burden and the opportunity for early intervention in emergency settings.
Beyond physical health, alcohol misuse impairs work performance through absenteeism, presenteeism, and diminished decision-making. Warning signs relevant to professionals include drinking alone, generous pours at home, daily pre-bed drinks, and alcohol affecting work or relationships. These patterns, when recognized early, can prompt timely intervention.
Evidence-Based Interventions for Employers and Individuals
Employers in Atlanta’s professional sector can take concrete steps to reduce alcohol misuse and support recovery:
- Implement universal screening and brief intervention. Use validated tools like the AUDIT-C in occupational health programs and employee wellness initiatives. Provide confidential referral pathways to evidence-based treatment.
- Develop gender-responsive programming. Tailor messaging and resources for midlife women, emphasizing alcohol-cancer links and heightened susceptibility to liver disease. Adjust program timing to accommodate caregiving schedules.
- Modify social norms. Offer alcohol-free networking events. Ensure that client entertainment budgets include robust non-alcohol options. Signal leadership support for low- or no-alcohol choices to reduce social pressure.
- Address co-use. Integrate smoking and vaping cessation supports within alcohol misuse programming, given the strong linkage between nicotine use and high-intensity binge drinking among adults aged 40–64.
Clinical and health system actions include systematic screening in primary care for adults aged 45–64, with brief counseling and pharmacotherapy where appropriate. Emergency departments should expand brief intervention protocols for alcohol-involved visits and link patients to outpatient treatment and workplace employee assistance programs.
Policy levers proven to reduce excessive alcohol use include increasing alcohol taxes and reducing outlet density or hours. The CDC explicitly recommends these strategies to curb alcohol-attributable mortality.
For individuals seeking to reduce intake, practical tools include tracking pours, setting drink limits, and identifying triggers. Accountability structures, peer support, digital tools, or clinician partnership, can reinforce behavior change. Heavy daily drinkers should seek medical supervision when reducing consumption, given withdrawal risks.
Surveillance and Monitoring Recommendations
Stakeholders in Atlanta should build a local monitoring dashboard that combines multiple data streams:
- OASIS ER trends. Quarterly updates of age 45–64 alcohol-related ER visit rates, sex-stratified, for Atlanta-area counties. Display deduplicated counts to assess unique patient burden.
- BRFSS benchmarks. Use Atlanta MSA SMART BRFSS 2012–2015 estimates for the 45–64 age group as historical context, and track Georgia statewide adult binge prevalence from 2016 onward to inform directionality.
- National context. Update CDC alcohol-attributable mortality rates annually, displaying chronic versus acute proportions to anchor chronic disease messaging.
- Environmental indicators. Track Atlanta MSA employment in food services and drinking places as a proxy for venue availability, and overlay with employer policy adoption metrics.
- Equity lens. Disaggregate by sex and, where possible, race and ethnicity to identify subgroups at increased risk.
This multi-level approach respects the strengths and limitations of each data source while providing actionable intelligence for intervention planning.

Conclusion: A Call to Action
Triangulating national mortality and emergency department trends, age-specific behavioral patterns, Georgia’s surveillance capacity, and Atlanta’s post-pandemic hospitality rebound, the evidence suggests that alcohol misuse among middle-aged professionals in the Atlanta area increased during 2019–2021 and remains a significant health and occupational risk.
Chronic conditions drive the majority of alcohol-attributable deaths, and women face disproportionate harm. The imperative now is to translate these insights into targeted, gender-responsive screening and prevention strategies within Atlanta’s professional workplaces and clinical systems, supported by policy levers that reduce excessive alcohol use.
If you or someone you know is struggling with alcohol misuse, confidential support is available. Reach out to Summit Wellness Group’s addiction counseling to explore evidence-based treatment options personalized to your needs.
