Choosing between fluoxetine and Zoloft for obsessive-compulsive disorder can feel overwhelming when intrusive thoughts and compulsions already consume your day.
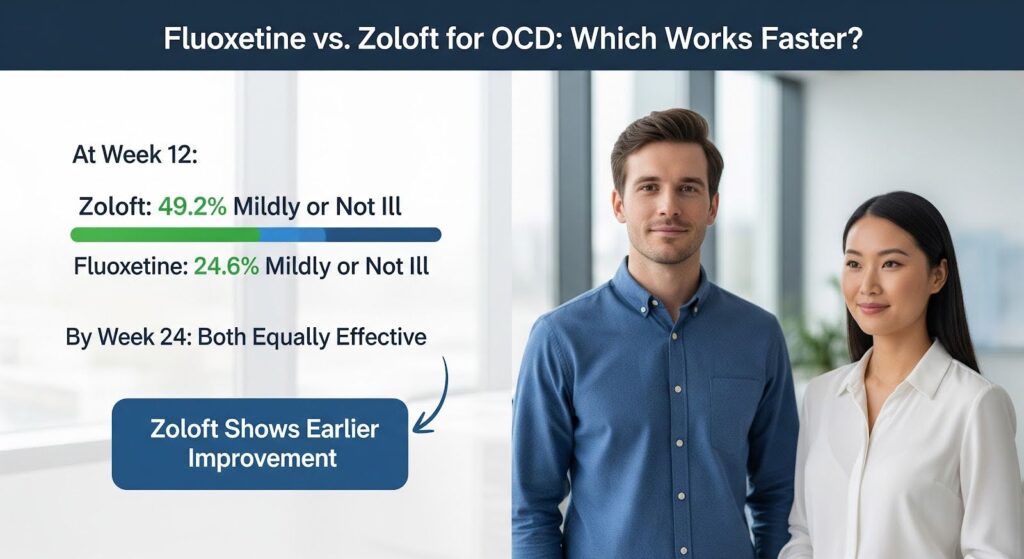
Both medications are FDA-approved SSRIs that help reduce OCD symptoms, and a 24-week clinical trial found them equally effective by the end of treatment, though Zoloft showed earlier improvement at 12 weeks with 49.2% of patients rated mildly or not ill compared to 24.6% on fluoxetine.
This article breaks down the evidence on efficacy, dosing, side effects, and discontinuation to help you and your doctor make the right choice for your situation.
Understanding How Fluoxetine and Zoloft Work for OCD?
Both fluoxetine and Zoloft belong to the selective serotonin reuptake inhibitor class. They work by blocking the serotonin transporter, which increases serotonin availability in brain circuits involved in OCD. This mechanism helps reduce the intensity and frequency of obsessions and compulsions over time.
The key difference lies in their pharmacokinetics. Fluoxetine has a long half-life, meaning it stays in your system for weeks after you stop taking it. This creates a gradual washout and reduces withdrawal symptoms if you miss doses. Zoloft has a shorter half-life, which allows for more flexible dose adjustments but requires more careful tapering when discontinuing.
Drug interactions also differ significantly. Fluoxetine strongly inhibits the CYP2D6 enzyme, which can interfere with many other medications. Zoloft has a more favorable interaction profile, making it easier to manage if you take multiple medications. The American Psychiatric Association notes this practical advantage when selecting between SSRIs for complex cases.
Comparing Effectiveness: Fluoxetine vs Zoloft for OCD
Head-to-Head Trial Results
The most direct comparison comes from a double-blind study that followed 150 adults with moderate to severe OCD for 24 weeks. Researchers randomly assigned 77 patients to Zoloft and 73 to fluoxetine, measuring outcomes on the Yale-Brown Obsessive Compulsive Scale and other standard measures.
By week 24, both medications produced equivalent and significant improvement on all primary measures. However, the timeline of improvement differed. At week 12, nearly half of Zoloft-treated patients were rated mildly ill or not ill on the Clinical Global Impression scale, compared to about one quarter of fluoxetine patients. This difference reached statistical significance.
Remission rates also favored Zoloft at the 12-week mark, with 20% achieving remission compared to 8% on fluoxetine. By week 24, the gap narrowed but remained numerically higher for Zoloft at 36% versus 22%. Both medications were well tolerated throughout the study.
Dose-Response Patterns
OCD typically requires higher SSRI doses than depression. A meta-analysis of fixed-dose trials found that higher doses of SSRIs produce better efficacy in OCD, with the strongest dose-response relationship seen for fluoxetine. Patients taking 60 to 80 mg fluoxetine equivalents showed greater symptom reduction than those on medium or low doses, though higher doses also increased dropout rates due to side effects.
The dose-response signal for Zoloft appears less steep in fixed-dose studies, but clinical experience shows many patients need 150 to 200 mg daily for optimal benefit. A randomized trial in Zoloft nonresponders found that escalating from 200 mg to 250 to 400 mg daily produced faster symptom improvement with similar side effect rates, supporting careful dose escalation in resistant cases.
Time to Initial Benefit
Improvement in OCD takes longer than in depression. Initial benefits may not appear until 4 to 6 weeks, and adequate trials typically require at least 12 weeks at near-maximal tolerated doses. The trajectory of SSRI action shows separation from placebo can be detected by week 2, but clinically meaningful functional change develops gradually.
This delayed response pattern makes the earlier improvement signal with Zoloft clinically relevant. If you need to engage in exposure and response prevention therapy or return to work quickly, those extra weeks of symptom relief at the 12-week mark may matter significantly.
Dosing Strategies for Optimal Results
Adult Dosing Guidelines
For adults with OCD, treatment guidelines emphasize escalating to effective doses within 4 to 6 weeks and maintaining that dose for at least 6 to 8 additional weeks before declaring nonresponse. The American Psychiatric Association guidelines recommend this approach across all SSRIs.
Fluoxetine dosing:
- Start at 20 mg daily
- Increase to 40 mg after 1 to 2 weeks
- Target range: 40 to 80 mg daily for OCD
- Allow 1 to 2 weeks between dose increases
- Full trial: 12 weeks at target dose
Zoloft dosing:
- Start at 50 mg daily
- Increase by 50 mg weekly or biweekly as tolerated
- Target range: 150 to 200 mg daily for OCD
- Consider 250 to 400 mg in resistant cases with monitoring
- Full trial: 12 weeks at target dose
Pediatric Dosing Considerations
Both medications are FDA-approved for pediatric OCD. Zoloft is approved from age 6, while fluoxetine is approved from age 7. Pediatric dosing requires more gradual titration and careful monitoring for activation symptoms.
A 13-week pediatric trial of fluoxetine used an algorithm starting at 10 mg daily, increasing to 20 mg after 2 weeks, with optional 20 mg increases at weeks 4 and 7 up to 60 mg daily. This systematic approach produced significant improvement compared to placebo with similar discontinuation rates.
For Zoloft, children ages 6 to 12 typically start at 25 mg daily, while adolescents start at 50 mg daily. Doses are increased by 25 to 50 mg increments weekly or biweekly to a target of 100 to 200 mg daily as tolerated.

| Medication | Adult Starting Dose | Adult Target Range | Pediatric Starting Dose | Pediatric Target Range |
|---|---|---|---|---|
| Fluoxetine | 20 mg daily | 40–80 mg daily | 10 mg daily | 20–60 mg daily |
| Zoloft | 50 mg daily | 150–200 mg daily | 25–50 mg daily | 100–200 mg daily |
Side Effects and Tolerability
Common Adverse Effects
A network meta-analysis across SSRIs and SNRIs for anxiety and OCD found that medication groups had higher overall adverse event rates than placebo. However, Zoloft and fluoxetine stood out as exceptions, not showing significantly higher overall adverse event rates than placebo in pooled analyses.
Both medications can cause nausea, insomnia or drowsiness, sexual dysfunction, tremor, and sweating. Higher doses increase the likelihood and intensity of these effects. In adults, these side effects are generally manageable with dose adjustments and supportive care.
Pediatric Safety Concerns
In children and adolescents, SSRIs increase activation symptoms like restlessness and insomnia compared to placebo. A Bayesian meta-analysis of pediatric SSRI trials in anxiety and OCD found increased rates of activation, insomnia, sedation, abdominal pain, headaches, and adverse event-related discontinuation versus placebo.
Importantly, treatment-emergent suicidality was not increased for SSRIs in pediatric OCD and anxiety trials. This finding provides reassurance, though close monitoring remains essential during the first weeks of treatment and around dose changes.
Cardiac Safety
Unlike citalopram and escitalopram, which carry regulatory warnings about QT interval prolongation and maximum dose limits, fluoxetine and Zoloft show minimal clinically significant QTc changes at therapeutic doses. This makes them safer choices for OCD, where high doses are often needed.
Discontinuation and Withdrawal Considerations
Half-Life Impact on Withdrawal
Fluoxetine’s long half-life substantially reduces discontinuation symptoms. A randomized interruption study simulating missed doses found that fluoxetine-treated patients experienced significantly fewer discontinuation-emergent events than those on Zoloft or paroxetine. Fluoxetine patients also had less reemergence of depressive symptoms during the interruption.
This pharmacokinetic advantage makes fluoxetine more forgiving if you miss doses and easier to discontinue when the time comes. Zoloft requires gradual tapering to minimize withdrawal symptoms, and even slow tapers may not fully prevent discontinuation effects.
Relapse Risk After Stopping Treatment
A systematic review of relapse prevention trials in anxiety disorders, OCD, and PTSD found that discontinuing antidepressants increased relapse odds more than threefold compared to continuation. Relapse prevalence was 36.4% in the placebo group versus 16.4% in those who continued medication over 8 to 52 weeks.
These findings underscore that OCD requires long-term therapy. Most guidelines recommend maintaining effective SSRI treatment for 1 to 2 years after achieving remission before considering a gradual taper. Combining medication discontinuation with ongoing exposure and response prevention therapy helps prevent relapse.
Integrating Medication with Cognitive Behavioral Therapy
Exposure and response prevention therapy is highly effective for OCD. A systematic review of pediatric OCD treatments found that adding CBT to SSRI treatment substantially improved outcomes, while adding SSRI to high-quality ongoing CBT yielded little additional short-term benefit.
For moderate to severe OCD, combination therapy typically outperforms medication alone. The earlier symptom relief that Zoloft may provide at 12 weeks can help you engage more effectively in exposure exercises, especially if severe symptoms have been limiting your ability to participate in therapy.
Which Medication Should You Choose?
When Zoloft May Be Preferred
Zoloft holds practical advantages for many adults with OCD:
- You take multiple medications and need to avoid drug interactions
- Earlier global improvement at 12 weeks matters for your work or therapy engagement
- Your doctor wants flexibility to escalate beyond 200 mg if needed
- You prefer shorter time between dose adjustments
The head-to-head trial showing higher remission rates at 12 weeks and the high-dose escalation data supporting doses up to 400 mg daily in resistant cases make Zoloft a rational first choice for many patients.
When Fluoxetine May Be Preferred
Fluoxetine offers distinct benefits in certain situations:
- You or a family member responded well to fluoxetine previously
- You have concerns about missing doses or discontinuation symptoms
- You want a medication with a strong dose-response signal to guide escalation
- Your doctor plans to optimize to 60 to 80 mg daily
The long half-life reduces withdrawal risk and makes fluoxetine more forgiving of inconsistent adherence. The dose-response meta-analysis showing clearer benefit at higher fluoxetine doses supports aggressive optimization when tolerated.
Pediatric Considerations
Both medications work well in children and adolescents with OCD. Zoloft’s FDA approval from age 6 and straightforward titration framework make it an excellent first choice. Fluoxetine remains a strong alternative, particularly when adherence patterns favor a long half-life or when there is prior positive response.
A 16-week pediatric trial found that fluoxetine showed no superiority at 8 weeks but significant benefit by week 16, with 57% much or very much improved compared to 27% on placebo. This delayed time course means you need to allow at least 12 to 16 weeks for full effects in young patients.
Making the Decision Work for You
The choice between fluoxetine and Zoloft matters less than ensuring you receive an adequate trial at an effective dose for at least 12 weeks. Both medications are sound first-line options with comparable endpoint efficacy when properly optimized.
Success depends on several factors beyond medication selection:
- Escalating to high therapeutic doses within 4 to 6 weeks
- Maintaining that dose for at least 6 to 8 additional weeks
- Integrating exposure and response prevention therapy
- Monitoring for side effects and adjusting as needed
- Planning for long-term maintenance to prevent relapse
Work closely with your doctor to track your symptoms using standardized measures like the Yale-Brown Obsessive Compulsive Scale. Define clear response thresholds, typically a 25 to 35% reduction in symptoms, and remission goals before starting treatment. This objective approach helps you and your treatment team make informed decisions about dose adjustments, augmentation, or switching if needed.
If you’re struggling with OCD and need comprehensive support that combines medication management with evidence-based therapy, consider reaching out for Summit’s dual diagnosis treatment that addresses both your OCD symptoms and any co-occurring mental health concerns.
