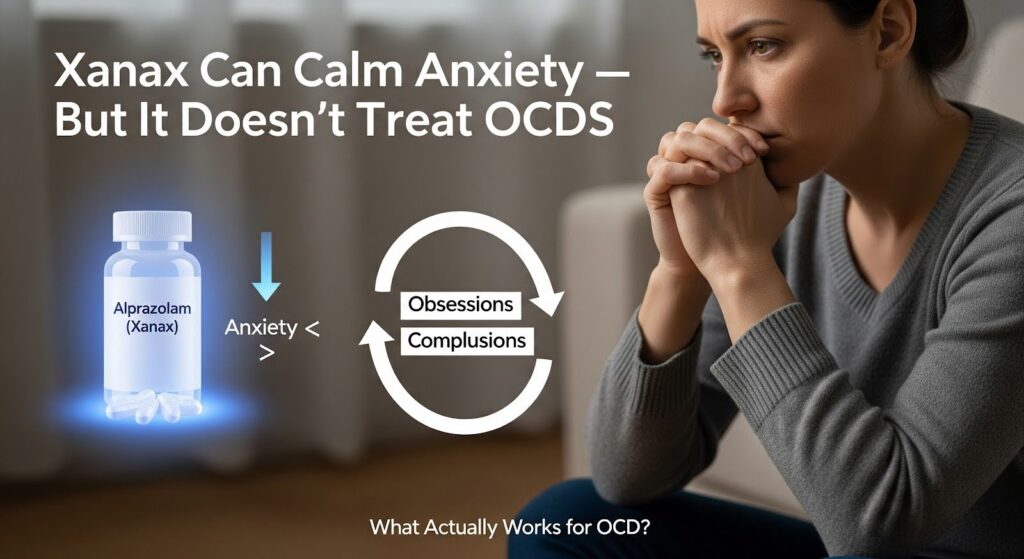
If you’re struggling with intrusive thoughts and repetitive behaviors, you may wonder whether Xanax can help. While alprazolam (Xanax) can reduce the anxiety that often accompanies obsessive-compulsive disorder, controlled trials show it does not meaningfully improve core OCD symptoms like obsessions and compulsions.
This article explains why benzodiazepines rarely help OCD, what treatments actually work, and when short-term Xanax use might be considered.
What is OCD and How is it Measured?
Obsessive-compulsive disorder affects roughly 2 to 3 percent of the population. The condition is marked by unwanted, intrusive thoughts, images, or urges (obsessions) and repetitive behaviors or mental acts (compulsions) performed to reduce distress.
Clinicians measure severity using the Yale-Brown Obsessive-Compulsive Scale, a 10-item tool scored from 0 to 40. Scores of 16 to 23 indicate moderate OCD, while 24 to 31 signals severe symptoms.
The disorder stems from dysfunction in brain circuits linking the orbitofrontal cortex, anterior cingulate, and striatum. These networks control habit formation and threat evaluation. When they misfire, people get stuck in loops of intrusive worry and ritualized responses.
Effective treatments directly recalibrate these circuits through learning-based therapy or serotonin-targeting medications, not through general anxiety suppression.
Does Xanax Help With OCD Thoughts?
No. The best available evidence indicates Xanax does not reduce obsessions or compulsions. A randomized controlled trial tested clonazepam, a benzodiazepine similar to alprazolam, against placebo in 27 people with OCD over 10 weeks.
Clonazepam showed no advantage on any measure, including obsession severity, compulsion frequency, or overall symptom scores. Only one of 16 patients on clonazepam met response criteria, compared to two of nine on placebo.
An older study compared clomipramine, alprazolam, and placebo. Clomipramine produced a 50 percent response rate, while alprazolam’s 18 percent response mirrored placebo’s 19 percent. This stark difference underscores that Xanax lacks meaningful anti-obsessional effects.
Why Xanax Feels Helpful but Isn’t?
Patients often report feeling calmer on Xanax. The drug enhances GABA-A receptor signaling, producing rapid anxiolysis and sedation. This can make intrusive thoughts feel less overwhelming in the moment.
However, the frequency and intensity of obsessions typically do not change, and the drive to perform compulsions persists. Any short-term relief may reinforce avoidance rather than promote the corrective learning needed for recovery.
What Treatments Actually Work for OCD?
Exposure and Response Prevention (ERP)
ERP is the gold-standard psychotherapy for OCD. This specialized form of cognitive behavioral therapy systematically exposes you to feared situations or thoughts while preventing ritualized responses. Over time, your brain learns that feared outcomes do not occur or can be tolerated. Numerous trials show ERP is superior to control conditions and at least as effective as medications, with enduring benefits.
When added to antidepressants, ERP often boosts outcomes. In one randomized trial, ERP augmentation outperformed risperidone augmentation in people who had partial responses to serotonin reuptake inhibitors. ERP works by engaging extinction learning in brain circuits linking the amygdala and prefrontal cortex, directly addressing the maladaptive habits that drive OCD.
SSRIs and Clomipramine
Serotonin reuptake inhibitors are first-line medications for OCD. Unlike major depression, OCD typically requires high-end dosing and at least 12 weeks at the maximum tolerated dose before determining response. Meta-analyses confirm SSRIs outperform placebo, and higher doses are more effective than medium or low doses.
Clomipramine, a potent serotonin reuptake inhibitor, shows superior efficacy over SSRIs in some analyses, though it carries more side effects. Both medication classes modulate serotonergic tone in the brain circuits that malfunction in OCD, enabling plasticity and reducing overvaluation of threat.
Augmentation for Treatment-Resistant OCD
Approximately 40 to 60 percent of patients do not achieve adequate relief with a single SSRI trial. For these individuals, evidence supports several augmentation strategies:
- Antipsychotic medications: Risperidone, aripiprazole, and haloperidol outperform placebo when added to SSRIs in treatment-resistant OCD. Quetiapine and olanzapine do not show superiority.
- Glutamatergic agents: Memantine and N-acetylcysteine show promise in randomized trials for moderate to severe OCD, though more research is needed.
- Intensified ERP: Adding or intensifying exposure therapy often produces better outcomes than medication augmentation alone.
Benzodiazepines do not appear in evidence-based augmentation algorithms for OCD.
Can Xanax Help OCD in Any Situation?
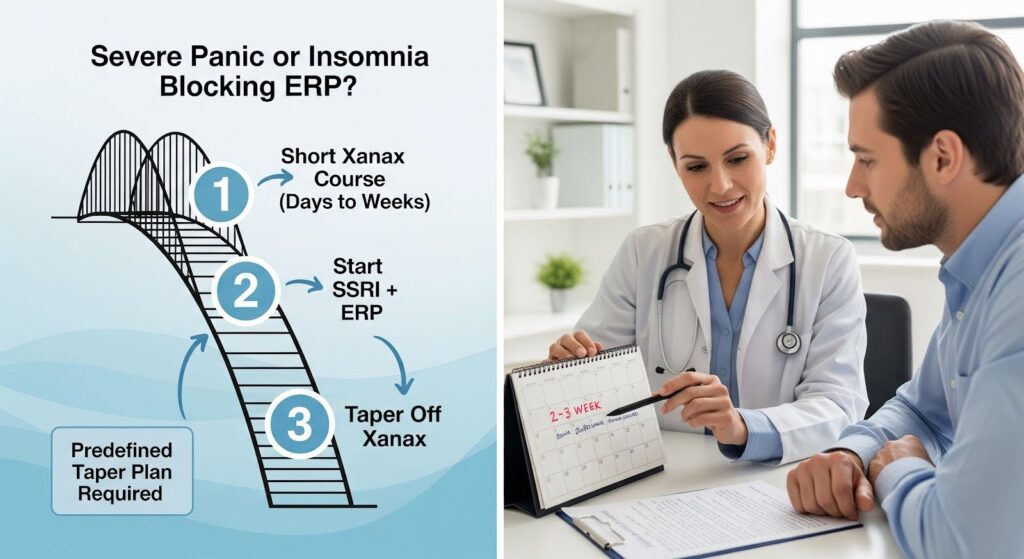
A narrow, time-limited role may exist for Xanax in highly selected cases. If severe panic attacks or insomnia prevent you from starting ERP or tolerating SSRI initiation, a clinician might consider a short course of alprazolam as a bridge. This approach requires:
- Lowest effective dose for the shortest possible duration, typically days to a few weeks maximum
- Avoidance of dosing before or after ERP sessions, since benzodiazepines can blunt the learning processes central to exposure therapy
- A predefined taper plan to minimize withdrawal, rebound anxiety, and dependence
- Close monitoring for tolerance, cognitive slowing, and falls
Even in this scenario, non-benzodiazepine alternatives and behavioral strategies should be prioritized. The clinical focus must remain on high-dose SSRIs and expert-delivered ERP.
Why Benzodiazepines May Interfere With ERP?
ERP relies on fear extinction, a learning process mediated by NMDA receptor-dependent plasticity in the amygdala and prefrontal cortex. Benzodiazepines enhance inhibitory signaling broadly, which can reduce the mismatch between expected and actual threat needed for learning.
Translational studies show that benzodiazepines given early in extinction training can impair acquisition and retention of extinction memories in animal models.
In humans, this suggests that taking Xanax around exposure sessions may undermine therapeutic gains. Over time, reliance on benzodiazepines may entrench avoidance rather than promote tolerance of distress, the very skill ERP aims to build.
Risks of Long-Term Benzodiazepine Use
OCD is often a chronic condition requiring months to years of sustained treatment. Benzodiazepines carry well-documented risks that accumulate over time:
| Risk | Description |
|---|---|
| Dependence and withdrawal | Chronic use produces receptor-level changes and behavioral dependence; abrupt discontinuation can trigger rebound anxiety and withdrawal syndrome |
| Cognitive impairment | Meta-analyses show long-term users exhibit deficits in working memory, processing speed, and divided attention; partial recovery may occur after tapering but can take months |
| Psychomotor impairment | Increased risk of falls, traffic accidents, and injuries, especially in older adults |
| Interaction risks | Respiratory depression when combined with opioids; amplified sedation with alcohol or other sedatives |
Given these risks and the lack of efficacy for core OCD symptoms, benzodiazepines have a poor risk-benefit ratio in this population.
What Do Guidelines Recommend?
Modern treatment guidelines from the World Federation of Societies of Biological Psychiatry specify SSRIs and ERP as first-line for OCD. Clomipramine is second-line due to side effects. Augmentation with antipsychotics or other agents is reserved for SSRI nonresponders.
Benzodiazepines are not recommended for core OCD symptoms and, at most, considered for very short-term adjunctive use to help acute distress or insomnia during SSRI initiation.
The International College of Obsessive-Compulsive Spectrum Disorders emphasizes that benzodiazepines have limited efficacy for OCD, do not show benefit when combined with SSRIs specifically for OCD symptoms, and carry dependence risks that make them unsuitable for long-term use.
Does Xanax Help With OCD and Panic Disorder?
Some people with OCD also experience panic disorder. Benzodiazepines do show short-term efficacy for panic attacks, with response rates roughly 1.6 times higher than placebo.
However, the evidence quality is low, and concerns about withdrawal, dependency, and uncertain long-term benefit mean SSRIs and cognitive behavioral therapy remain preferred first-line treatments for panic.
If you have both OCD and panic, a clinician might consider a brief benzodiazepine course to control acute panic while initiating SSRI and arranging ERP. This does not mean Xanax treats your OCD. It addresses a comorbid condition that could otherwise prevent engagement with effective OCD therapies.
Practical Steps for OCD Treatment
If you are considering treatment for OCD, follow this evidence-based pathway:
1. Get an accurate diagnosis: A clinician will assess severity using the Yale-Brown scale, screen for comorbid conditions like panic or tics, and evaluate functional impact.
2. Start ERP and an SSRI: Initiate exposure therapy with a trained therapist and begin an SSRI, titrating to the high-end recommended dose as tolerated. Set expectations for an 8 to 12 week onset.
3. Avoid routine benzodiazepines: Resist the temptation to use Xanax for OCD thoughts. If used for acute panic or insomnia, document a clear taper plan and avoid dosing around ERP sessions.
4. Evaluate nonresponse: After at least 12 weeks at maximum SSRI dose, consider intensifying ERP, switching to clomipramine, or adding an antipsychotic like risperidone or aripiprazole.
5. Maintain effective therapy: Continue treatment to prevent relapse. Maintenance pharmacotherapy reduces relapse risk; discuss gradual tapering only after sustained remission.
Why the Brain Science Matters?
OCD involves hyperactivity and dysconnectivity in circuits linking the orbitofrontal cortex, anterior cingulate, and striatum. These networks control habit formation and goal-directed behavior. Deep brain stimulation targeting these circuits can ameliorate severe, refractory OCD, underscoring their causal role.
ERP and SSRIs directly recalibrate these systems through learning-based plasticity and serotonergic modulation. Benzodiazepines, by contrast, enhance GABA signaling broadly without specifically addressing the learning computations or habit loops that drive OCD.
This mechanistic mismatch explains why Xanax provides transient anxiolysis but does not change the disorder’s core.
Our Evidence-Based Position
Based on the totality of evidence, alprazolam should not be used as a treatment for core OCD symptoms. It lacks randomized trial support, can impair extinction learning essential for ERP, and carries well-characterized risks that are particularly problematic in a chronic disorder.
The only potentially defensible role is a tightly controlled, very short-term adjunct for severe acute comorbid panic or insomnia during SSRI initiation, employed at the lowest effective dose, separated from ERP sessions, and limited to days to a few weeks with a predefined taper.
Even in this narrow role, non-benzodiazepine alternatives and behavioral strategies should be prioritized. Clinicians must explicitly counsel about dependence, cognitive effects, driving risks, and the plan to discontinue. The clinical effort should remain squarely focused on high-dose, adequately timed SSRIs or clomipramine, expert-delivered ERP, and evidence-based augmentation strategies when needed.
Finding the Right Support
OCD is a challenging condition, but effective treatments exist. If intrusive thoughts and compulsions are disrupting your life, you deserve care that addresses the root of the problem, not just the anxiety on the surface. Combining evidence-based therapy with the right medication can help you reclaim control and build lasting recovery.
Reach out to Summit because we specialize in dual diagnosis treatment to explore a personalized plan that works for you.
