If intrusive thoughts and repetitive behaviors are disrupting your daily life, you’re likely searching for relief that actually works.
Sertraline, commonly known as Zoloft, is one of the most widely prescribed medications for obsessive–compulsive disorder, with multiple randomized controlled trials showing it reduces OCD symptoms more effectively than placebo, often by 16% or more on standard rating scales within 12 weeks.
This article will walk you through how Zoloft works for OCD, what doses are most effective, how quickly you can expect results, and how it compares to other treatment options.
How Zoloft Works for OCD?
Zoloft belongs to a class of medications called selective serotonin reuptake inhibitors (SSRIs). These drugs increase serotonin levels in the brain by blocking the serotonin transporter, which normally removes serotonin from the space between nerve cells. For people with OCD, this boost in serotonin appears to help regulate the brain circuits involved in obsessive thoughts and compulsive behaviors.
What makes OCD different from conditions like depression is that it typically requires higher SSRI doses to achieve meaningful symptom relief. Research consistently shows a dose–response relationship in OCD: higher doses produce greater symptom reduction and higher response rates. This pattern is unique to OCD and doesn’t appear as clearly in major depressive disorder, suggesting that the underlying brain mechanisms differ between these conditions.
Clinical Evidence: Does Zoloft Actually Help With OCD?
Multiple high-quality studies confirm that Zoloft reduces OCD symptoms significantly compared with placebo. In one large multicenter trial involving 325 adults, participants taking Zoloft showed a 16.2% reduction in Yale–Brown Obsessive–Compulsive Scale (Y-BOCS) scores, while those on placebo improved by only 6.55%. The responder rate, meaning people who experienced clinically meaningful improvement, was more than double in the Zoloft group (25.6%) compared with placebo (11.4%).
Long-term studies paint an equally encouraging picture. In a one-year fixed-dose trial, people who responded to Zoloft at doses of 50 or 200 mg per day maintained their improvements over an additional 40 weeks. Both the lower and higher doses significantly outperformed placebo on all investigator-rated scales, and the medication remained well tolerated throughout the year-long study period.
When to Expect Results?
You won’t need to wait months to know if Zoloft is working. Clinical improvement often becomes noticeable within 2 to 6 weeks, with the most substantial gains typically appearing by week 12. In fixed-dose studies, separation from placebo emerged as early as week 3 on both symptom scales and global improvement ratings.
Early response is also predictive. If you experience at least a 20% reduction in symptoms by week 4 after reaching a therapeutic dose, you have a good chance of achieving a full response by week 12. Conversely, if you see minimal improvement by weeks 4 to 6, it may be time to discuss dose adjustments or alternative strategies with your provider.
Optimal Dosing: How Much Zoloft for OCD?
Standard Dosing Range
The FDA-approved dose range for Zoloft in OCD is 50 to 200 mg per day. Most people start at 50 mg daily and increase by 50 mg increments each week as tolerated. Clinical experience and research suggest that many adults with OCD need 150 to 200 mg per day to achieve adequate symptom control.
A rapid titration study found that reaching 150 mg per day by day 5 produced faster symptom reductions at weeks 4 and 6 compared with slower titration to the same dose by day 15, without increasing side effects or dropout rates. This suggests that, for some people, getting to a therapeutic dose quickly can speed relief.
High-Dose Strategies for Nonresponders
What if you’ve tried 200 mg per day for several weeks and still aren’t seeing enough improvement? A pivotal multicenter trial offers important guidance. Researchers took 66 adults who hadn’t responded after 16 weeks on 50 to 200 mg per day and randomized them to either continue at 200 mg or escalate to 250 to 400 mg daily for 12 more weeks.
The high-dose group, averaging about 357 mg per day, showed significantly greater and faster improvement on Y-BOCS scores, global OCD ratings, and clinician-rated improvement scales. Importantly, adverse event rates were similar between the two groups, with insomnia, diarrhea, nausea, headache, and fatigue being the most common side effects in both arms.
While categorical responder rates didn’t differ dramatically at the 12-week endpoint, the high-dose approach accelerated symptom reduction and deepened overall improvement. This suggests that for people who tolerate Zoloft well but remain symptomatic at standard doses, carefully monitored escalation above 200 mg per day is a valid and evidence-supported strategy.
Real-World Safety at Higher Doses
A 2024 retrospective study examined 105 adults with OCD treated with off-label high-dose serotonin reuptake inhibitors, including sertraline-equivalent doses up to 650 mg per day, for an average of 21 months. Side-effect rates did not differ significantly across low, moderate, and high-dose groups. The most common effects were sexual dysfunction (34%), weight gain (27%), sedation (26%), excessive sweating (19%), and tremor (10%).
Serious adverse events were rare: one abnormal ECG, one first-time seizure, and 4.8% with transient liver enzyme elevations. Critically, there were no cases of serotonin syndrome or drug-induced liver injury. All participants received routine ECG and lab monitoring, underscoring the importance of medical supervision when using higher doses.
Comparing Zoloft to Other OCD Treatments
Zoloft vs Other SSRIs
Zoloft’s effectiveness is comparable to other SSRIs like fluoxetine, fluvoxamine, paroxetine, and escitalopram. A comprehensive network analysis concluded that SSRIs, the older tricyclic antidepressant clomipramine, and cognitive behavioral therapy variants are all effective for adult OCD. Psychotherapies alone or combined with medications tend to produce greater effects than medications alone.
Zoloft has some practical advantages. Unlike citalopram, which carries dose-related heart rhythm risks, Zoloft has a relatively benign cardiac profile. It also has unique randomized trial data supporting escalation above 200 mg per day in nonresponders, an advantage when considering how far to push monotherapy before switching or adding other treatments.
The Role of Exposure and Response Prevention (ERP)
Exposure and response prevention therapy is the gold-standard psychotherapy for OCD. In a head-to-head augmentation trial involving SSRI partial responders, adding ERP outperformed adding the antipsychotic risperidone and placebo, improving both OCD symptoms and quality of life more robustly and without the metabolic and movement-related side effects of antipsychotics.
This finding is crucial: ERP should be your first augmentation strategy if Zoloft alone isn’t enough. Combining ERP with medication from the start generally produces better outcomes than medication alone, and intensifying ERP sessions is often more effective and safer than adding antipsychotic drugs.
Antipsychotic Augmentation
For people who don’t respond adequately to optimized SSRI doses plus ERP, antipsychotic augmentation can help. Risperidone (0.5 to 2 mg per day) and aripiprazole (10 to 15 mg per day) have the strongest evidence, with response rates around 50% within 4 to 6 weeks in selected patients.
However, antipsychotics carry risks including weight gain, metabolic changes, and movement disorders. They should be used judiciously, for limited periods, and discontinued if no benefit appears within 4 to 6 weeks or if side effects become problematic.

Emerging Options: Brain Stimulation
For SSRI-resistant OCD, repetitive transcranial magnetic stimulation (rTMS) and deep TMS are noninvasive brain stimulation techniques showing promise. Meta-analyses indicate that rTMS augmentation yields clinically meaningful Y-BOCS reductions and higher response odds versus sham stimulation, with acceptable tolerability. Deep TMS using specialized coils has shown encouraging results in pilot and multicenter studies, though larger fully blinded trials are still needed to refine protocols and patient selection.
Side Effects and Safety Considerations
Zoloft is generally well tolerated. The most common side effects include:
- Gastrointestinal upset (nausea, diarrhea)
- Insomnia or drowsiness
- Headache
- Sexual dysfunction
- Fatigue
These effects are typical of the SSRI class and often diminish after the first few weeks. In long-term studies, fewer than 20% of participants discontinued Zoloft due to adverse events.
Monitoring and Precautions
While Zoloft has a favorable safety profile, certain precautions apply:
- Serotonin syndrome: Rare but serious; risk increases when combining with other serotonergic drugs. Watch for agitation, confusion, rapid heart rate, high blood pressure, dilated pupils, muscle rigidity, and fever.
- Hyponatremia: Low sodium levels, especially in older adults. Symptoms include headache, confusion, weakness, and unsteadiness.
- Bleeding risk: SSRIs can increase bleeding risk, particularly when combined with NSAIDs, aspirin, or blood thinners.
- Seizure threshold: SSRIs may lower seizure threshold slightly; use caution in people with seizure disorders.
- Cardiac effects: Zoloft has minimal QTc prolongation risk compared with some other SSRIs, but ECG monitoring may be warranted in high-risk patients or those on interacting medications.
If you’re considering doses above 200 mg per day, routine monitoring, including ECG, liver enzymes, and metabolic panels, is standard practice to catch any issues early.
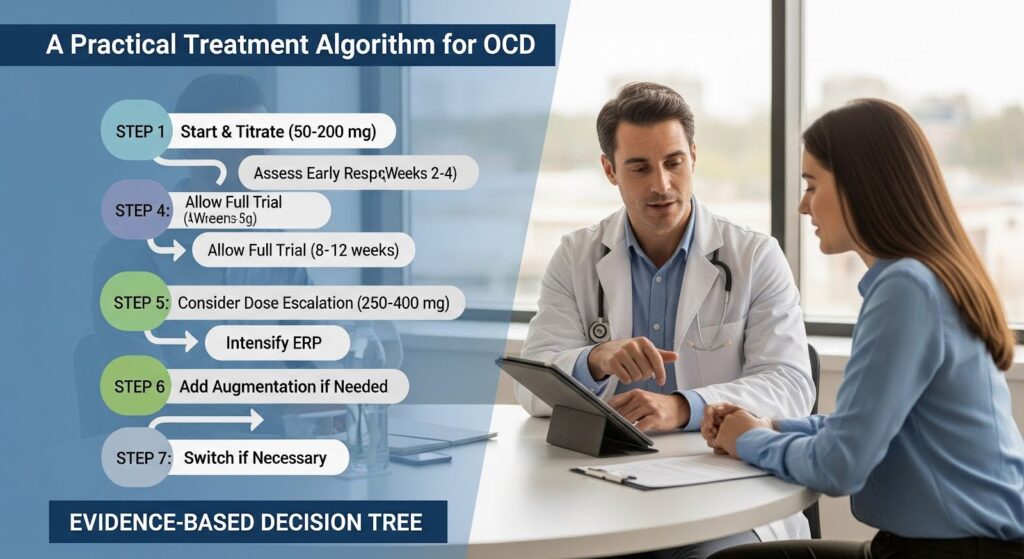
A Practical Treatment Algorithm
Based on the evidence, here’s a step-by-step approach to using Zoloft for OCD:
Step 1: Start and titrate
Begin at 50 mg per day and increase by 50 mg weekly as tolerated, aiming to reach 150 to 200 mg per day by weeks 3 to 5. Integrate ERP therapy as early as possible.
Step 2: Assess early response
Measure symptoms at 2 to 4 weeks after reaching a therapeutic dose. If you see at least 20% improvement, continue the current plan. If improvement is minimal and you’re not yet at 200 mg, optimize the dose promptly.
Step 3: Allow adequate trial duration
Continue for at least 8 to 12 weeks total, with 4 to 6 weeks at your maximum tolerated dose, before judging whether the medication is working.
Step 4: Consider dose escalation
If you tolerate Zoloft well but remain significantly symptomatic at 200 mg per day, discuss escalating to 250 to 400 mg per day with your provider. This requires close monitoring but can accelerate and deepen improvement.
Step 5: Intensify ERP
If response is partial, increase the frequency or intensity of ERP sessions before adding other medications. ERP augmentation often outperforms antipsychotic augmentation.
Step 6: Add augmentation if needed
For persistent partial response despite optimized Zoloft and ERP, consider short-term antipsychotic augmentation (risperidone or aripiprazole) or explore brain stimulation options like rTMS.
Step 7: Switch if necessary
If Zoloft fails despite high-dose optimization and ERP, switching to another SSRI at higher OCD doses or to clomipramine (with appropriate cardiac and plasma-level monitoring) may be warranted.
Key Takeaways
| Question | Answer |
|---|---|
| Does Zoloft help with OCD? | Yes. Multiple randomized trials show Zoloft reduces OCD symptoms significantly more than placebo, with benefits often appearing within 2 to 6 weeks. |
| What dose is most effective? | Most adults need 150 to 200 mg per day. For nonresponders who tolerate the medication, doses of 250 to 400 mg per day can provide additional benefit with careful monitoring. |
| How long until it works? | Early improvement often appears by weeks 2 to 4, with maximum benefit typically by week 12. |
| Is Zoloft safe long-term? | Yes. One-year studies show sustained benefit and good tolerability at doses of 50 to 200 mg per day. |
| What if Zoloft alone isn’t enough? | Prioritize adding or intensifying ERP therapy. If needed, antipsychotic augmentation or brain stimulation may help. |
| How does it compare to other treatments? | Zoloft is as effective as other SSRIs and can be combined with ERP for best results. ERP augmentation outperforms antipsychotic augmentation in head-to-head trials. |
Moving Forward With Confidence
Zoloft is a proven, flexible, and generally well-tolerated medication for OCD. The evidence supports an assertive approach: start therapy early, titrate to an adequate dose quickly, allow enough time at the maximum tolerated dose, and integrate ERP from the beginning. For people who don’t respond fully at standard doses, carefully monitored escalation above 200 mg per day is a valid, evidence-supported strategy that can accelerate improvement without significantly increasing safety risks.
The strongest outcomes come from combining medication with exposure and response prevention therapy. If you’re struggling with OCD and haven’t found relief yet, a comprehensive approach that includes optimized Zoloft dosing and evidence-based psychotherapy offers the highest probability of meaningful, lasting improvement.
If you or someone you care about is navigating OCD alongside substance use or co-occurring mental health challenges, specialized support can make all the difference. Reach out to explore Summit’s dual diagnosis treatment that addresses both conditions together.
